By the way, there are two recent meta-analyses. Zitterman 2012 (referenced by Michael) and Schöttker 2012 (below). The latter is more consistent with a slightly higher range of benefit, e.g. 30-
40ng instead of ~30ng/ml, but I haven't looked into any details.
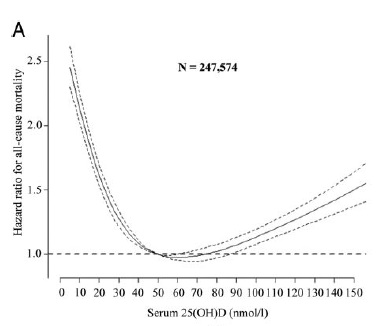
“There appeared to be a roughly inverse linear relationship of 25(OH)D levels and mortality in all studies except for the studies of Michaelsson et al., 2010, that observed a u-shaped association, and Cawthon et al., 2010, that found no association between 25(OH)D levels and all-cause mortality. For all other studies, the group with lowest 25(OH)D levels had the highest mortality risk. [but there seems to be no formal analysis of this?!]”
all-cause mortality reduced with a pooled
HR of 0.92 (95% confidence interval: 0.89-0.95) for a 20nmol/l increase in 25(OH)D levels.
“we only included population-based cohort studies addressing the outcome all-cause mortality, whereas the meta-analysis of Zittermann et al., 2012 included also studies with community-dwelling adults that do not reflect random population samples (over-sampling of subjects with ≥2 domains in disability in Semba et al., 2009, recruitment of ambulatory patients in Kuroda et al., 2009 and inclusion of high-risk patients for vitamin D deficiency because the vitamin D status was determined at the provider's discretion for clinical indications, like, e.g. osteoporosis, in Anderson et al., 2010), other study types (Bolland et al., 2010 reported on a trial of calcium supplementation) and another outcome (cardiovascular mortality in Kilkkinen et al., 2009).”
Ageing Res Rev. 2012 Feb 17. [Epub ahead of print]Serum 25-hydroxyvitamin D levels and overall mortality. A systematic review and meta-analysis of prospective cohort studies.
Schöttker B, Ball D, Gellert C, Brenner H.
Edited by kismet, 02 July 2012 - 11:56 PM.