S O U R C E : n a t u r e (ePDF)
ABSTRACT
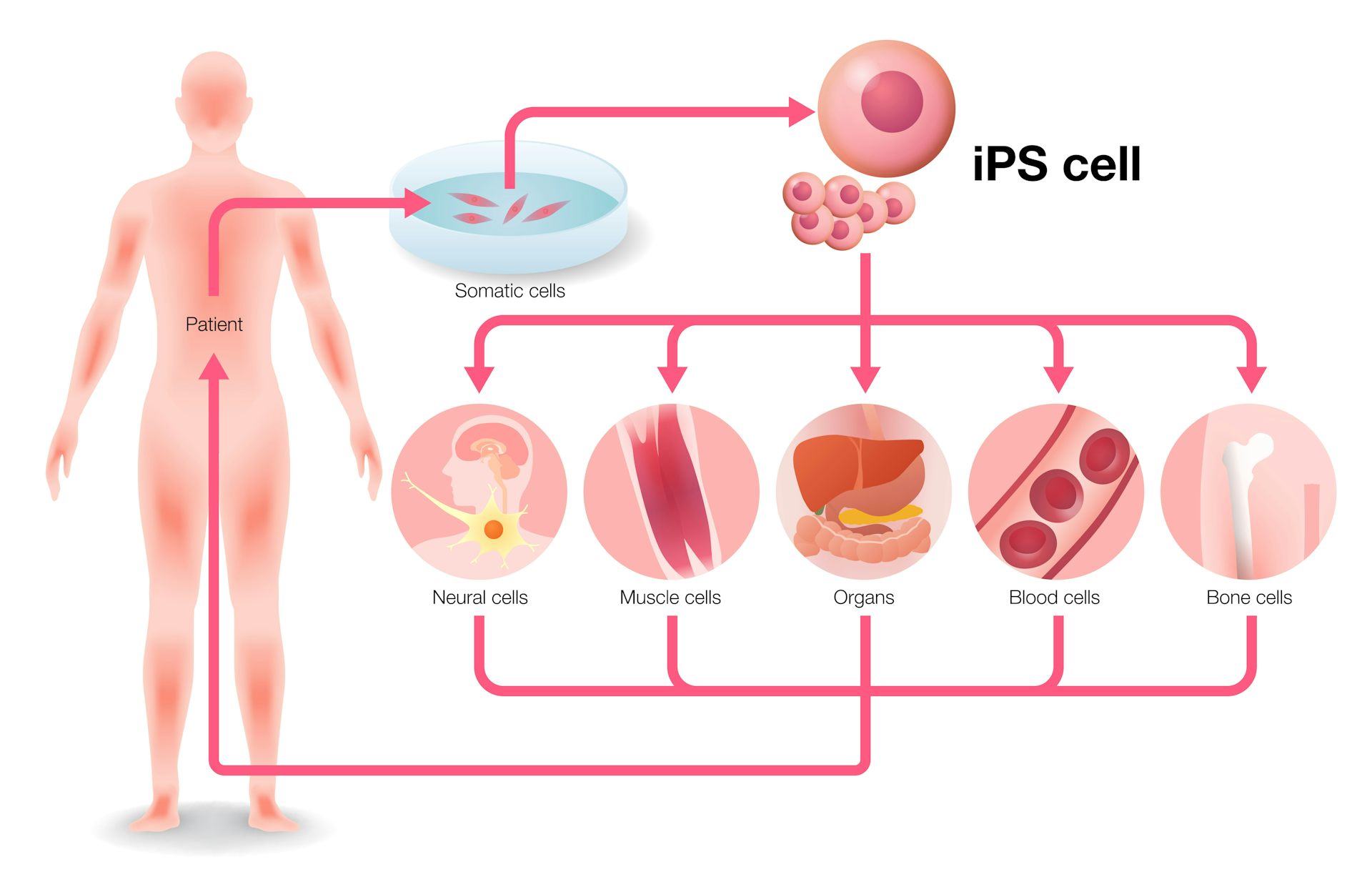
The utility of autologous induced pluripotent stem cell (iPSC) therapies for tissue regeneration depends on reliable production of immunologically silent functional iPSC derivatives. However, rejection of autologous iPSC-derived cells has been reported, although the mechanism underlying rejection is largely unknown. We hypothesized that de novo mutations in mitochondrial DNA (mtDNA), which has far less reliable repair mechanisms than chromosomal DNA, might produce neoantigens capable of eliciting immune recognition and rejection. Here we present evidence in mice and humans that nonsynonymous mtDNA mutations can arise and become enriched during reprogramming to the iPSC stage, long-term culture and differentiation into target cells. These mtDNA mutations encode neoantigens that provoke an immune response that is highly specific and dependent on the host major histocompatibility complex genotype. Our results reveal that autologous iPSCs and their derivatives are not inherently immunologically inert for autologous transplantation and suggest that iPSC-derived products should be screened for mtDNA mutations.
iPSC-derived grafts can be immunogenic and rejected by the host even though they are derived from host cells. Several factors relating to the reprogramming of somatic cells, expansion of iPSCs in culture and differentiation of iPSCs into tissue cells are thought to contribute. Suppression1 and overexpression2 of pluripotency factors are known to establish denovo antigenicity that diminishes with differentiation1,3,4. However, differentiation of iPSCs can lead to the expression of immunogenic antigens not usually expressed in corresponding somatic cells causing rejection.5 In addition, muta-tions acquired during reprogramming and expansion may generate mutant proteins that can act as neoantigens.Mutation rates during reprogramming have been reported to be up to ninefold higher than the background mutation rate in culture.6 Furthermore, the mutation rate for mtDNA is 10- to 20-fold higher than that of nuclear DNA7–9. Both mutated and wild-type mtDNA can coexist in the same cell, a phenomenon called heteroplasmy10. Nonsynonymous mtDNA mutations can impact both the function of proteins11 and its antigenicity. mtDNA-encoded mitochondrial minor antigens12 have been described as transplant barriers13, and our group has shown that individual single nucleotide polymor-phisms (SNPs) are sufficient to create immunogenic neoantigens14. However, the extent to which neoantigenic SNP enrichments affect autologous immune responses are not known. Here we sought to characterize the immunogenicity of mtDNA SNPs and assess their immunologic relevance for iPSC-based regenerative therapies.First, we assessed the sensitivity and specificity of the mouse immune system to respond to isolated mtDNA SNPs. Using the tech-nique of somatic cell nucleus transfer, embryonic stem cells (ESCs) with BALB/c (B/c) nuclear DNA and C57BL/6 (B6) mtDNA were generated (these cells are referred to as NT-ESCs throughout). In comparison to B/c, these NT-ESCs showed only two homoplasmic nonsynonymous SNPs in the mt-Co3 and mt-Cytb genes, and gen-erate cytochrome C oxidase III (Co3) or cytochrome b (Cytb) pro-teins with one amino acid substitution each (Supplementary Table 1). NT-ESCs were used for immunization against these two epitopes in B/c mice (Fig. 1a). To confirm that mitochondrial proteins with a single amino acid substitution can function as neoantigens, B/c fibroblasts were transfected to transiently overexpress either the B/c or B6 forms of Co3 or Cytb (Fig. 1a,b). Splenocytes recovered after 5 d were used for enzyme-linked immunospot (ELISpot) assays against either of the four fibroblast preparations. ELISpot assays for interferon-γ (IFN-γ) and interleukin-4 (IL-4) were performed.
Spot frequencies are presented to directly compare the immune response against the allogeneic B6 protein with that of the syngeneic B/c protein (Fig. 1c). Only the two fibroblasts overexpressing alloge-neic B6 protein evoked a substantial Tcell response. When trans-planted into B/c recipients (Fig. 1d), only those two fibroblast grafts underwent rejection (Fig. 1e,g) during the time period of protein overexpression (Fig. 1f,h). Mass cytometry of splenocytes recovered after 5 d revealed remodeling of the T and B cell compartments as Both high-passage iPSC lines from B6 and FVB revealed potential neoantigens. Single-cell sequencing of B6 cells showed that the heteroplasmies obtained in bulk sequencing accurately reflected the average of more heteroge-neous heteroplasmies in individual cells (Supplementary Table 9).The MHC binding affinities of the B6 neoantigen candidates were modeled using in silico prediction (Supplementary Fig. 8c and Supplementary Table 10), which showed that the mutant SNP in mt-Co1 generated peptides with decent MHC binding affinities whereas the affinity of the mutant Nd3 peptide was very low. Twenty-residue oligomers were synthesized from a sequence carrying the neoanti-genic or reference SNP (Supplementary Table 11). Mice were immu-nized with low-passage or high-passage iPSCs and splenocytes were challenged with 20-residue oligomers 5 d later (Supplementary Fig. 8d–f). As predicted, in B6 mice we observed IFN-γ and IL-4 responses against the Co1 neoantigen but not the mutant Nd3. Immunogenicity was also demonstrated for the 20-residue oligomer of the Atp8 neoantigen in FVB (Supplementary Fig. 8g–i).B6 (Fig. 3c–e) and FVB mice (Supplementary Fig. 9) then received subcutaneous grafts of either low-passage or high-passage iPSCs to assess whether the neoantigens could provoke an immune response and diminish cell survival invivo. Varying cell numbers were used, as the survival and teratoma formation of pluripotent cell grafts depends on the overall cell load16. Across graft sizes, we observed an increased immune response and a correspondingly reduced survival of high-passage iPSC grafts.
... / ...
F O R T H E R E S T O F T H E R E S E A R C H A R T I C L E, V I S I T T H E S O U R C E (.ePDF)