Scientists have found a way to directly stimulate the assembly of Complex I in mitochondria, rescuing memory deficits in mouse models of Alzheimer’s and frontotemporal dementia [1].
Mitochondrial signal transducers
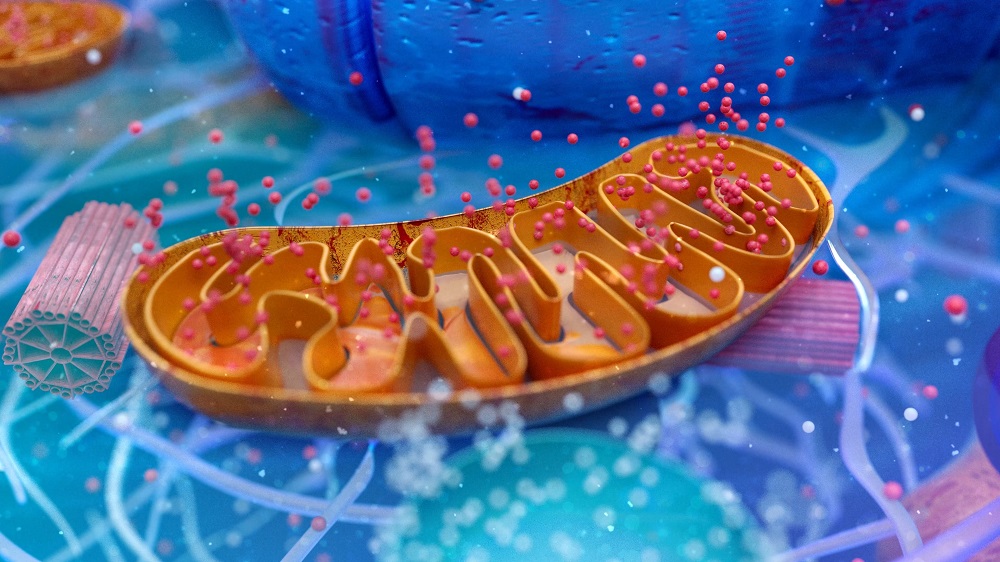
Many neurodegenerative diseases, such as Alzheimer’s disease, are associated with mitochondrial dysfunction [2], which might lead to cells not working properly or dying off. However, it’s been difficult to determine whether mitochondrial problems are a root cause or a symptom of these diseases.
This uncertainty exists mainly due to the lack of reliable ways to specifically and quickly boost mitochondrial function in the brain. In a new study published in Nature Neuroscience, researchers from Inserm and the Université de Bordeaux, in collaboration with researchers from the Université de Moncton in Canada, inched closer to answering the question and maybe developing therapies for mitochondrial disorders.
In previous studies, the researchers worked on the role of guanine nucleotide-binding proteins (G proteins). Their main role is signal transduction: they typically sit inside the cell’s main outer membrane, linked to G protein-coupled receptors (GPCRs). When a signaling molecule, such as a hormone or a neurotransmitter, binds to a GPCR on the cell surface, the receptor activates its associated G protein, which initiates a downstream cascade of biochemical reactions within the cell, leading to a specific physiological change.
However, recent studies have found that G proteins exist also in mitochondrial membranes and regulate energy production [3]. The researchers reasoned that activating G proteins directly inside the mitochondria could rapidly ramp up the organelles’ activity and improve cognitive function.
The tool they built to influence mitochondrial Gs protein (“s” for the stimulatory subtype) is based on Designer Receptor Exclusively Activated by Designer Drugs (DREADD) technology. A DREADD is a receptor protein that has been altered so that it no longer responds to its natural activators but can be switched on by a specific and otherwise inert “designer drug,” such as clozapine-N-oxide (CNO).
The researchers also attached a sequence to the construct that would guide it directly to mitochondria, ensuring that it does not end up in other membranes. Using high-resolution microscopy and protein analysis, they confirmed that the new tool was successfully delivered and embedded into the outer membrane of mitochondria in various cell types and in the hippocampi of mice.
A phosphorylation cascade triggers energy production
The experiments showed that activating mitoDREADD-Gs with CNO had a direct and rapid effect on mitochondrial function. In cells and hippocampal tissue expressing the tool, CNO treatment significantly increased mitochondrial membrane potential, which is an indicator of energy-producing activity, and oxygen consumption rate (OCR), which directly measures mitochondrial respiration. The team also used a control DREADD that wasn’t targeted to the mitochondria, and it had no such effect.
“This work is the first to establish a cause-and-effect link between mitochondrial dysfunction and symptoms related to neurodegenerative diseases, suggesting that impaired mitochondrial activity could be at the origin of the onset of neuronal degeneration,” said Giovanni Marsicano, Inserm research director and co-senior author of the study.
The researchers also confirmed that mitoDREADD-Gs works by activating the naturally present (endogenous) Gs protein. When cells genetically engineered to lack Gs were used, the tool failed to boost mitochondrial activity.
Investigating the entire mechanism, the team found that the mitochondrial Gs protein triggered a cascade of phosphorylation, starting with the enzyme protein kinase A (PKA). The ultimate target turned out to be NDUFS4, a component of Complex I of the electron transport chain, the machinery in the heart of mitochondrial energy production, promoting its assembly and activity.
Memory rescued in mice
The researchers then turned to two mouse models: one of of frontotemporal dementia (FTD) and another Alzheimer’s disease. They first confirmed that these mice had lower mitochondrial respiration and reduced PKA activity in the hippocampus, a brain region critical for memory.
In both models, when mitoDREADD-Gs was expressed in the hippocampi of these mice and activated with CNO, the animals’ performance in novel object recognition (NOR), a common memory test in rodent studies, was fully restored to the level of healthy mice. The control (non-mitochondrial) DREADD had no effect.
“These results will need to be extended, but they allow us to better understand the important role of mitochondria in the proper functioning of our brain. Ultimately, the tool we developed could help us identify the molecular and cellular mechanisms responsible for dementia and facilitate the development of effective therapeutic targets,” said Étienne Hébert Chatelain, professor at the Université de Moncton and co-senior author of the study.
“Our work now consists of trying to measure the effects of continuous stimulation of mitochondrial activity to see whether it impacts the symptoms of neurodegenerative diseases and, ultimately, delays neuronal loss or even prevents it if mitochondrial activity is restored,” added Luigi Bellocchio, Inserm researcher and co-senior author of the study.
Literature
[1] Pagano Zottola, A. C., Martín-Jiménez, R., Lavanco, G., Hamel-Côté, G., Ramon-Duaso, C., Rodrigues, R. S., … & Hebert-Chatelain, E. (2025). Potentiation of mitochondrial function by mitoDREADD-Gs reverses pharmacological and neurodegenerative cognitive impairment in mice. Nature Neuroscience, 1-14.
[2] Wang, W., Zhao, F., Ma, X., Perry, G., & Zhu, X. (2020). Mitochondria dysfunction in the pathogenesis of Alzheimer’s disease: recent advances. Molecular neurodegeneration, 15(1), 30.
[3] Suofu, Y., Li, W., Jean-Alphonse, F. G., Jia, J., Khattar, N. K., Li, J., … & Friedlander, R. M. (2017). Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release. Proceedings of the National Academy of Sciences, 114(38), E7997-E8006.
View the article at lifespan.io