A recent study investigated plasma proteins in people exposed to secondhand smoke and found that exposure affected multiple molecular processes, including immune, inflammatory, and tissue repair pathways [1].
Carrying the consequences of something you didn’t do
It is widely known and researched that smoking is bad for health, and there are even similarities between smoking and aging on the molecular level. However, second-hand smoke, despite affecting around one third of the population [2], appears to get less attention, even though it’s also bad for human health and has been linked to 1.2 million deaths per year among non-smokers [3]. In non-smokers, second-hand smoke was also linked to developing coronary artery disease, lung cancer cases, breast cancer, chronic obstructive pulmonary disease (COPD), and diabetes [2, 4].
A broader look
To better understand the molecular mechanism underlying second-hand smoke’s systemic impact on health, the researchers investigated all the plasma proteins (the proteome) of 48 healthy restaurant workers occupationally exposed to second-hand smoke. They conducted an initial study on those same workers previously reporting on the impact of second-hand smoking on nasal epithelial cells, which showed changes in levels of various proteins involved in oxidative stress and cell detoxification. This time, they aimed to investigate “global protein expression changes in plasma” following exposure to second-hand smoke.
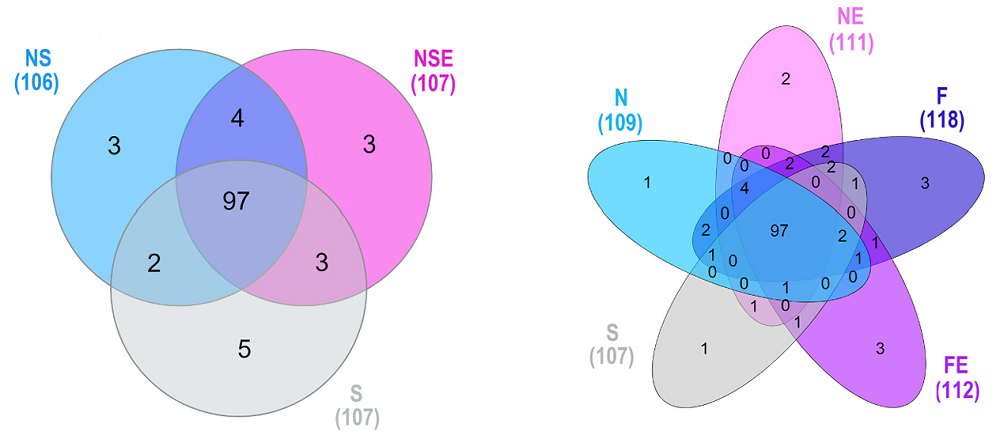
The researchers divided the cohort into three main categories: Non-Smokers (NS), Non-Smokers Exposed (NSE), and Current Smokers (S), or into five subgroups: Never Smokers (N), Never Smokers Exposed (NE), Former Smokers (F), Former Smokers Exposed (FE), and Current Smokers (S). The authors analyzed differentially expressed proteins across those groups, with the restriction that proteins had to be detected in at least 80% of each group or subgroup.
The researchers highlighted several proteins and functions that were differentially expressed across subgroups. This data showed that processes linked to immunity, inflammatory responses, gene transcription, autophagy, blood transport, mTORC1 signalling, and protein breakdown, among others, were impacted by smoking and secondhand smoke.
Focusing on single proteins
The researchers also discussed specific proteins identified in their analysis, including those that showed the most significant differences in expression across groups, and suggested the possible impact of those proteins on people exposed to second-hand smoke. They found that one of the proteins whose levels were increased in such people is butyrylcholinesterase (BChE), an enzyme that can neutralize toxic compounds. The authors suggest that increased levels of this protein can be “a compensatory detoxification response.”
Another protein that had reduced levels in the plasma of the Never and Former Exposed subgroups is Vitamin D-binding protein (GC), which is essential for vitamin D transport and clearance of actin. The researchers hypothesized that exposure to second-hand smoke “may lead to epithelial injury and actin release into circulation, increasing the demand for these scavenger proteins.”
Vitamin D-binding protein also plays a role in inflammatory processes; therefore, this result suggests that there is endothelial inflammation in smokers and people exposed to second-hand smoke. This is unsurprising, as previous research also linked second-hand smoke exposure to increased levels of systemic inflammatory markers [5]. This study, besides Vitamin D-binding protein, identified eight more inflammation-related proteins linked to second-hand smoke, strengthening the evidence of its pro-inflammatory effects.
Because of these proteomic results, the researchers proposed that second-hand smoke exposure might disrupt the clearance of cellular debris, modulate the immune system, and reduce the capacity for tissue repair. These disruptions contribute to tissue damage, chronic inflammation, or autoimmune-like responses.
The researchers also note that previous research has linked “mild systemic inflammation coupled with cellular debris from cell death” to cardiovascular disease [6]. Earlier research also showed secondhand smoke to induce acute atherothrombosis, that is, the formation of a blood clot on atherosclerotic plaque that leads to such conditions as heart attack or stroke.
The current study also shows links between those processes and secondhand smoke. For example, in the Never Smokers Exposed, Former Smokers, and Former Smokers Exposed groups, they identified an increased level of the protein alpha-2-antiplasmin (SERPINF2), which plays an essential role in blood clotting, making secondhand-exposed people more prone to blood clotting. Elevated levels of this protein have previously been linked to atherosclerosis and thrombosis risk [7].
Another protein, whose low levels have previously been linked to poor outcomes in cardiovascular disease [8], apoA4, was downregulated in the Non-Smokers Exposed group.
Those are only a few examples, and the researchers briefly discuss a few more, some of which are linked to insulin signaling, thyroid hormones, or immune function, indicating that second-hand smoke dysregulates multiple molecular processes.
Possible biomarkers
The researchers conclude that exposure to second-hand smoke was associated with changes in protein expression that are linked to the “response to toxic elements in the blood, systemic inflammation/autoimmunity, and blood vessel diseases.” Long-term follow-up to detect changes over time would provide more answers about how second-hand smoke affects health in the long term. Still, even this small study provides valuable information on possible changes. It also helps identify protein signatures that can aid in developing biomarkers to assess the health risks associated with second-hand smoke.
Literature
[1] Neves, S., Pacheco, S. A., Vaz, F., Valentim-Coelho, C., Saraiva, J., James, P., Simões, T., & Penque, D. (2025). Second-hand smoke exposure modulates plasma proteins linked to detoxification, inflammation and atherothrombosis. Environmental toxicology and pharmacology, 120, 104864. Advance online publication.
[2] Flor, L. S., Anderson, J. A., Ahmad, N., Aravkin, A., Carr, S., Dai, X., Gil, G. F., Hay, S. I., Malloy, M. J., McLaughlin, S. A., Mullany, E. C., Murray, C. J. L., O’Connell, E. M., Okereke, C., Sorensen, R. J. D., Whisnant, J., Zheng, P., & Gakidou, E. (2024). Health effects associated with exposure to secondhand smoke: a Burden of Proof study. Nature medicine, 30(1), 149–167.
[3] GBD 2019 Risk Factors Collaborators (2020). Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England), 396(10258), 1223–1249.
[4] Daylan, A. E. C., Miao, E., Tang, K., Chiu, G., & Cheng, H. (2023). Lung Cancer in Never Smokers: Delving into Epidemiology, Genomic and Immune Landscape, Prognosis, Treatment, and Screening. Lung, 201(6), 521–529.
[5] DiGiacomo, S. I., Jazayeri, M. A., Barua, R. S., & Ambrose, J. A. (2018). Environmental Tobacco Smoke and Cardiovascular Disease. International journal of environmental research and public health, 16(1), 96.
[6] Ząbczyk, M., Ariëns, R. A. S., & Undas, A. (2023). Fibrin clot properties in cardiovascular disease: from basic mechanisms to clinical practice. Cardiovascular research, 119(1), 94–111.
[7] Humphreys, S. J., Whyte, C. S., & Mutch, N. J. (2023). “Super” SERPINs-A stabilizing force against fibrinolysis in thromboinflammatory conditions. Frontiers in cardiovascular medicine, 10, 1146833.
[8] Peng, J., & Li, X. P. (2018). Apolipoprotein A-IV: A potential therapeutic target for atherosclerosis. Prostaglandins & other lipid mediators, 139, 87–92.
View the article at lifespan.io








































