Today's interesting news, doing the rounds in the popular press and being gleefully misinterpreted along the way, is that, working in mice, researchers have induced temporarily increased levels of the proteins used to reprogram normal cells into pluripotent stem cells. This produced a number of short term benefits to regeneration and metabolism, though the long-term results on life span remain to be assessed. Cancer and regeneration are two sides of the same coin, and it is thought that the characteristic decline in stem cell activity with age is part of an evolved balance between risk of cancer and risk of tissue failure. Many of the methods of globally spurring greater regeneration either definitely or theoretically carry the risk of cancer. Stem cell therapies and telomerase gene therapies fall into this categories, though on the whole the cancer risk in practice has so far turned out to be lower than the cancer risk in theory. The reasons for this remain to be fully explored. Nonetheless, the whole complex system of a few stem cells with unlimited replication supporting a tissue of many somatic cells with tightly limited replication that exists in near all species came into being in the evolutionary context of cancer. We depend upon biological structures that are self-repairing and resilient in many ways, but that are very vulnerable to cellular malfunctions of uncontrolled growth that distort the structure and disrupt correct function. So where we are less self-repairing and resilient than we might be, cancer is the first and most obvious culprit when considering the evolutionary history that created us.
It has been a decade since researchers first figured out how to reprogram normal adult cells into induced pluripotent stem cells, capable of forming any cell, but likely to do who knows what if put into the context of living tissue. Reprogramming occurs in a cell culture, using a cell sample, not in a living organism. This reprogramming actually involves surprisingly few changes, dialing up the gene expression of a few specific proteins, with the first attempts using Oct4, Sox2, cMyc, and Klf4. The use of induced pluripotent stem cells in medicine is a matter of developing a methodology that will differentiate the pluripotent cells into the desired type of stem or progenitor cell appropriate to the tissue in question, using the patient's own cells as a starting point so that the resulting therapeutic cells are matched perfectly. That is fairly safe, given suitable testing, and will eventually provide a cost-effective source of all the cells needed for the next generation of regenerative medicine and tissue engineering. The cells put in place match those already present in the tissue, and should pick up on the same environment of signals and undertake the appropriate work of regeneration. Delivering pluripotent stem cells as-is, on the other hand, is just asking for cancer: it is more or less the same thing as putting precancerous cells into the patient. There is no control or guidance, and what happens next is up to the hand of fate.
Given this, one would think that taking the next step and using gene therapy to upregulate the reprogramming proteins in a living individual would be even worse. In addition to a whole bunch of newly pluripotent cells, you have newly pluripotent cells appearing in random locations and changed from random cells with random levels of preexisting damage. None of this sounds particularly safe. In fact, that experiment has been carried out in mice, and as you might expect the result is the development of cancers. The newly created pluripotent cells start building whatever springs to mind, wherever they happen to be. However, there are several examples we can point to in which dialing up protein production permanently is disastrous, but turning it up intermittently is quite beneficial. One good example is the tumor suppressor gene p53, which if producing proteins all the time will, in addition to even more effectively reducing cancer risk, accelerate aging by suppressing processes that are also necessary to regeneration and tissue maintenance. Cancer and regeneration use the same mechanisms - one is simply more regulated than the other. Most of the tumor suppression genes that have been cataloged target these shared mechanisms. Yet producing additional p53 only when regulatory processes determine it is needed, suppresses cancer more effectively without accelerating aging.
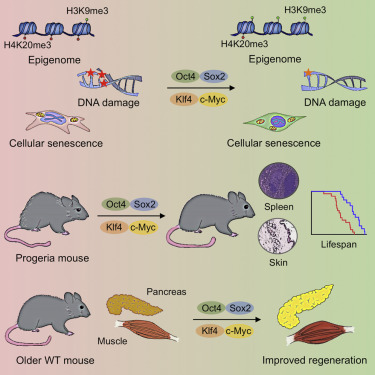
In this context the researchers here use a methodology of temporarily increasing expression of the pluripotency genes Oct4, Sox2, cMyc, and Klf4 in mice. They do this in cell cultures, then in mice with an accelerated aging disorder - actually a dysfunction of the cellular structure akin to that in human progeria - and then in normal aged adult mice. I think it a good idea to ignore the first two of these. Cell cultures are not living animals, and we should usually pay little attention to studies on accelerated aging models for the same reason we should pay little attention to studies in poisoned mice. Progeria and poisoning are both conditions that have little relevance to normal aging, being an accumulation of cell damage that doesn't occur to any large degree in normal aging, so it is often very hard to determine whether or not the results are in any way useful. If you produce a lot of damage and then help work around that damage, but none of the above actually happens in the course of ordinary aging, what does that say? The answer depends on details specific to each case that most of us are not knowledgeable enough to assess.
Fortunately here the researchers did undertake a study in normal mice. Unfortunately it was only a short-term study, so considerations of life span and longer term outcomes, such as cancer rate, will have to wait. Still, as an additional data point in the larger picture of what can be done to enhance regeneration in mammals, it is interesting. We can consider all sorts of plausible candidate mechanisms that have been explored in past years and likely overlap with those involved in the outcomes produced by stem cell transplants and telomerase gene therapies. That said, this upregulation of pluripotency factors is certainly something that I'd put in the "very unwise" bucket, should you find yourself in the position to undergo such a gene therapy in the years ahead. It is much more risky than telomerase gene therapy, and that in and of itself looks like something to skip until more data on the outcomes in larger mammals arrives.
Turning back time: Salk scientists reverse signs of aging
As people in modern societies live longer, their risk of developing age-related diseases goes up. In fact, data shows that the biggest risk factor for heart disease, cancer and neurodegenerative disorders is simply age. One clue to halting or reversing aging lies in the study of cellular reprogramming, a process in which the expression of four genes known as the Yamanaka factors allows scientists to convert any cell into induced pluripotent stem cells (iPSCs). Like embryonic stem calls, iPSCs are capable of dividing indefinitely and becoming any cell type present in our body. "What we and other stem-cell labs have observed is that when you induce cellular reprogramming, cells look younger. The next question was whether we could induce this rejuvenation process in a live animal."
While cellular rejuvenation certainly sounds desirable, a process that works for laboratory cells is not necessarily a good idea for an entire organism. For one thing, although rapid cell division is critical in growing embryos, in adults such growth is one of the hallmarks of cancer. For another, having large numbers of cells revert back to embryonic status in an adult could result in organ failure, ultimately leading to death. For these reasons, the team wondered whether they could avoid cancer and improve aging characteristics by inducing the Yamanaka factors for a short period of time. To find out, the team turned to a rare genetic disease called progeria. Both mice and humans with progeria show many signs of aging including DNA damage, organ dysfunction and dramatically shortened lifespan. Moreover, the chemical marks on DNA responsible for the regulation of genes and protection of our genome, known as epigenetic marks, are prematurely dysregulated in progeria mice and humans. Importantly, epigenetic marks are modified during cellular reprogramming.
Using skin cells from mice with progeria, the team induced the Yamanaka factors for a short duration. When they examined the cells using standard laboratory methods, the cells showed reversal of multiple aging hallmarks without losing their skin-cell identity. Encouraged by this result, the team used the same short reprogramming method during cyclic periods in live mice with progeria. The results were striking: Compared to untreated mice, the reprogrammed mice looked younger; their cardiovascular and other organ function improved and - most surprising of all - they lived 30 percent longer, yet did not develop cancer. Lastly, the scientists turned their efforts to normal, aged mice. In these animals, the cyclic induction of the Yamanaka factors led to improvement in the regeneration capacity of pancreas and muscle. In this case, injured pancreas and muscle healed faster in aged mice that were reprogrammed, indicating a clear improvement in the quality of life by cellular reprogramming.
In Vivo Amelioration of Age-Associated Hallmarks by Partial Reprogramming
The last decade of scientific research has dramatically improved our understanding of the aging process. The notion that cells undergo a unidirectional differentiation process during development was proved wrong by the experimental demonstration that a terminally differentiated cell can be reprogrammed into a pluripotent embryonic-like state. Cellular reprogramming to pluripotency by forced expression of the Yamanaka factors (Oct4, Sox2, Klf4, and c-Myc [OSKM]) occurs through the global remodeling of epigenetic marks.
Although in vitro studies have been informative, the physiological complexity of the aging process demands an in vivo approach to better understand how reprogramming may affect cellular and organismal aging. Breakthrough studies have shown that cellular reprogramming to pluripotency, although associated with tumor development (e.g., teratoma formation), can be achieved in vivo in mice by the forced expression of the Yamanaka factors. In addition, we and other groups have demonstrated that partial reprogramming in vitro by transient expression of OSKM can induce a dedifferentiated progenitor-like state. Together, these observations suggest that cellular reprogramming may be used to promote tissue regeneration and led us to hypothesize that in vivo partial reprogramming could slow or reverse the aging process and extend organismal lifespan. Here, we report that cyclic in vivo induction of OSKM in a mouse model of premature aging improves age-associated phenotypes and extends lifespan. In addition, we demonstrate the amelioration of cellular phenotypes associated with aging by short-term induction of the Yamanaka factors in mouse and human cells. Finally, we show that short-term expression of OSKM alleviates pancreatic and muscle injury in older wild-type (WT) mice.
Our observations may reinforce the potential role of epigenetic changes as drivers of aging and highlight the plasticity of the aging process, which might be altered by cellular reprogramming in vivo. In addition, our results suggest that aged cells undergo a process of molecular rejuvenation during the initial stages of cellular reprogramming to pluripotency. Failure to erase critical hallmarks of aging may lead to refractory populations of cells and cellular senescence. Due to the complexity of the reprogramming and aging processes, future studies will be necessary to investigate whether partial reprogramming can ameliorate aging hallmarks during physiological aging and to better understand the molecular mechanisms behind this phenomenon. This information will be necessary if we are to develop accurate and efficient epigenetic remodeling strategies toward maximizing the beneficial effects of in vivo reprogramming while avoiding potential risks associated with the in vivo expression of the Yamanaka factors.
Reading the whole of the analysis in the paper, I have to say that I think these researchers have a lot of the picture back to front. Putting epigenetic changes front and center as a primary mechanism in aging, as opposed to a reaction to rising levels of cell and tissue damage, is the cart in front of the horse. Sure, those epigenetic changes cause further problems, but focusing on targeting them won't remove the primary damage that causes aging. It only forces the damaged engine to work harder. Maybe that produces benefits, as it seems to in stem cell therapies that work via signaling to put existing cells back to work, but it isn't solving the real problem.
View the full article at FightAging