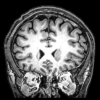
I've been doing some research on schizophrenia and the brain, also using ChatGPT to test the relevance of some of my ideas when it comes to the pathology.
NMDA-dysfunction is the core of schizophrenic brain abnormalty. What causes this dysfunction is elevated levels of Kynurenic acid (KYNA), a tryptophan metabolite that is an endogenous NMDA-antagonist.
-
Postmortem studies show increased KYNA in brains of schizophrenia patients.
-
CSF measurements reveal higher KYNA levels in living patients.
-
Animal studies link raised KYNA with schizophrenia-like behaviors.
-
Pharmacological interventions that reduce KYNA (e.g., KAT II inhibitors) are being explored as potential treatments.
The NMDA-antagonism causes the downstream effect of dopamine excess and other neurotransmitter abnormalties.
What also supports the NMDA-dysfunction hypothesis:
- NMDA-antagonist dissociative drugs like Ketamine and PCP mimic schizophrenia symptoms more accurately than any other models
- NMDA-agonists treat schizophrenia symptoms
- Clozapine is the superior antipsychotic because it releases glutamate and D-serine, which are endogenous NMDA-agonists
What causes the elevated levels of Kynurenic acid?
-
Abnormalities in the kynurenine pathway during brain development (e.g., in utero) might predispose individuals to schizophrenia later.
-
Stress, inflammation, or maternal infection can shift tryptophan metabolism toward more KYNA production.
Most often first episode psychosis is triggered by a traumatic event, chronic stress, drug abuse or physical illness. In these situations the person may feel unable to operate in the rational prefrontal thinking-planning-executing manner and is incapacitated which triggers dissociation as a primal mechanism to an overwhelming situation. The neurochemical that makes this dissociation possible is Kynurenic acid.
What can be done?
"Ways to lower KYNA include direct enzyme inhibition (KAT II inhibitors), pathway rebalancing (KMO activators), reducing inflammation, and lifestyle changes like exercise that divert kynurenine metabolism. Most pharmacological options are still experimental, but lifestyle and anti-inflammatory approaches are practical today."
Medications and supplements that target the NMDA-receptors - while they don't lower KYNA levels they treat the malfunction that it causes.
- Clozapine is the heavy artillery in schizophrenia treatment as explained earlier, it is the only known antipsychotic that treats the glutamatergic dysfunction. Unfortunately it has the side effects of atypical antipsychotics because of the antagonism of several different receptors and also the rare neutropenia risk so Clozapine should usually only be used if other medications and therapies fail. Clozapine is also a GABA-B agonist which is anxiolytic and the metabolite norclozapine is delta-opioid agonist which is antidepressive, contributing to its therapeutic effects.
- Sarcosine is a co-agonist of NMDA at the glycine site
- Theanine is a partial co-agonist at NMDA receptors
- D-aspartic acid is NMDA receptor full agonist
- Panax Ginseng seems to have modulatory effects at the NMDA-receptor and in studies decreases flat affect in schizos (most likely through 5-HT2A agonism)
- Bacopa Monnieri modulates NMDA-receptor function and has some evidence base of treating cognitive dysfunction in schizophrenia
- Pregnenolone is a positive allosteric modulator of NMDA-receptors
Kynurenic acid is also antagonist of the nicotinic acetylcholine receptors which causes cognitive deficits. No wonder the majority of schizophrenics self-medicate with Nicotine. The cholinergic system seems to deal with raw information received from surroundings so targeting this pathway can help as seen with the novel antipsychotic muscarinic agonist Cobenfy.
This is still quite simplified theory as there are various factors that influence the pathophysiology of schizophrenia and as seen in the Open Dialogue Model schizophrenia can be treated without resorting to antipsychotic medications at all. The key seems to be to deprogram this chronically maladaptive Kynurenic acid/dissociative pathway from the brain and the individual by providing safe environment and more healthy coping mechanisms to stress or other triggers. Current long-term antipsychotic medications as sole treatment most often result in poor life quality because they don't target the core of NMDA-dysfunction and usually also worsen negative symptoms of the disease by blocking dopamine and serotonin receptors in a forceful manner making normal neurotransmitter firing impossible.
Feel free to comment or share your ideas concerning this devastating yet fascinating disease. ![]()