This topic touches close to home, as I've probably spent the bulk of my research time on atopic dermatitis (eczema). I don't suffer from it, but my significant other does. By research time, I mean I've spent large amounts of time reading papers and learning about the immune system. I am not a doctor or an immunologist for that matter, just an engineer. But I feel I have a good understanding of the disease and I would like to share my findings. I apologize in advance as this is probably going to be a long post. References will be at the bottom.
In order to find supplements to help with eczema I found it incredibly helpful to understand how the disease works. This also aided me in looking out for which supplements to avoid.
The first thing to stress is: atopic dermatitis is not an autoimmune disease. Your body is not attacking itself. AD is a hypersensitivity to allergens and environmental irritants, characterized by two phases. An acute phase of intense itch and a chronic phase resulting of inflamed skin lesions caused by the mechanical trauma of itching. The mechanical trauma leads to a defective skin barrier, allowing bacteria and allergens to continue provoking an allergic reaction. AD is self reinforcing this way.
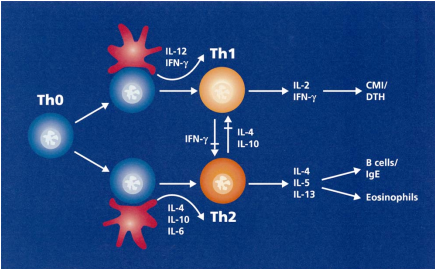
T Helper Cells, a sub-group of lymphocytes, are the key players in this disease. Naive T helper cells are differentiated into two subtypes, Th1 and Th2 cells. Th1 cells produce interferon gamma (IFN-y) and tumor necrosis factor (TNF) and also activate macrophages. Th2 cells produce several cytokines like IL-4, IL-5 and IL-13. These cytokines signal B lymphocytes to produce immunoglobulin E(IgE). IgE plays a key role in the acute itch of AD. IgE binds to mast cells and basophils. When IgE encounters an allergen, it causes mast cells to degranulate and release histamine (among other substances).
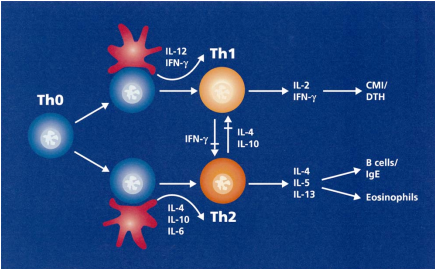
It is well accepted that AD's primary cause is an imbalance in Th1/Th2 cells, with a skew to Th2 cells. This leads to an increase in IL-4 and a hyperproduction of IgE. How this imbalance occurs is still not understood, but genetics and exposure to allergens at an early stage in life (or lack thereof) seem to play a role. Conventional treatment of AD is typically corticosteroids, which inhibit genes that code for cytokines like IL-4 and reduce T cell proliferation. The latest and greatest are calcineurin inhibitors. Calcineurin plays an important role in T cell differentiation.
So! How does this help in the search for supplements? One can seek out studies that involve:
- Up-regulating the Th1 response.
This should be approached with care, as a Th1 response is dominant in the chronic phase. - Reducing expression of IL-4
- Reducing serum IgE
- Studies that involve NC/Nga mice, a murine model specifically for AD. Another AD murine model are DS-Nh mice.
What have I found?
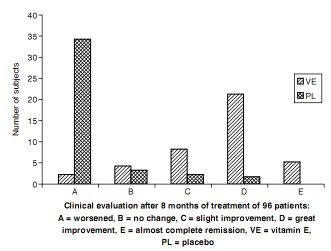
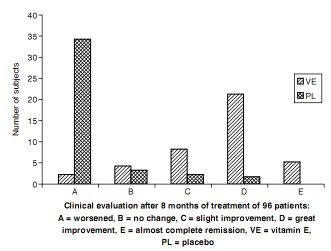
- Vitamin E: Tsoureli-Nikita et al. conducted a single blind, placebo controlled study of 96 participants treated with 400 IU of alpha tocopherol. Subjects that reported great improvement or complete remission showed a 62% drop in serum IgE. Here is a graph of how the participants responded.
Gamma-tocopherol also seems to have an effect on inflammatory cytokines. Wiser et al conducted an open label study of 16 volunteers, 8 non asthmatic and 8 asthmatic supplemented with 623 mg of gamma-tocopherol, 61.1 mg of alpha-tocopherol, 11.1 mg of beta-tocopherol and 231 mg of delta-tocopherol and found a significant (p<0.05) drop in IL-6, IL-1B, TNF-alpha. While the study did not address AD specifically, asthma is another atopic syndrome and is usually a comorbidity of AD. Based on these two main studies, I found a mixed tocopherols and tocotrienols supplement to be the best approach.
- Omega 3s (DHA): Koch et al. conducted a double blind, randomized, placebo controlled study of 53 subjects taking 5.4g of DHA daily for 8 weeks and and found a decrease in IgE synthesis. I do not have access to the research paper, so I don't know why DHA was the focus.
- Probiotic: Ghadimi et al. provided L. rhamnosus, L. gasseri, B. bifidum and B. longum to a small group of volunteers and found that they inhibited secretion of IL-4 and IL-5 (Th2) and stimulated IFN-y (Th1). In essence, they upregulated the Th1 response. Not a conclusive study by any means, but the only one I've found so far that studied probiotic effects on Th1/Th2 balance in-vivo.
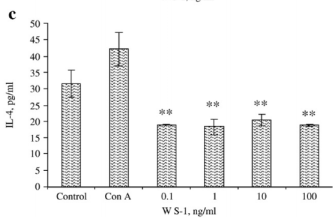
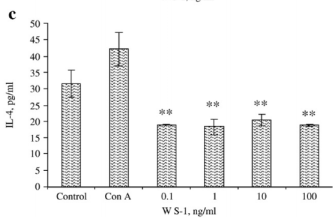
- Ashwagandha (Withania somnifera): Malik et al found that feeding BALB/c mice ashwagandha decreased IL-4 and upregulated a Th1 response. This IL-4 graph is what caught my eye.
- Gamma-linolenic acid (evening primrose, borage): I haven't done as much reading on y-linolenic acid.
This meta-analysis seems to indicate positive results.
This study seems to indicate that DGLA, what GLA is eventually converted to, prevents AD in NC/Nga mice.
Supplements to stay away from?
Anything that has a non specific upregulating effect on the immune system or a specific upregulation of Th2 cells. A specific example of this would be
melatonin. I know you are currently supplementing with resveratrol. I have no idea how resveratrol works on the immune system, but that would be something to look into.
Unless you are absolutely sure of the immune system effects of a supplement you are taking, stop taking it for a while and re-introduce to see if it triggers a flare up. I never thought melatonin could have immunomodulatory effects and it ended up causing a pretty significant AD flare in my significant other. We approach supplementation for her with a lot greater caution than I would for myself. We introduce a supplement one at a time, and allow a period of time to see if negatively affects her.
One last thing I would like to mention. Maintaining a healthy skin barrier is important in preventing flare ups.
Ceramides seem to play an important part in the stratum corneum. We have tried a cream with pseudo-ceramides called
CeraVe. This seems to be a the most effective cream so far, and believe me, our sample size of different creams is huge.
That's all I have.
References - a * denotes I have the full-text. If you are interested in reading it, PM me and I'll see about getting it to you.
General Atopic Dermatits Information
Abramovits W. Atopic dermatitis. J Am Acad Dermatol. 2005 Jul;53(1 Suppl 1):S86-93. *
Homey B, Steinhoff M, Ruzicka T, Leung DY. Cytokines and chemokines orchestrate atopic skin inflammation.J Allergy Clin Immunol. 2006 Jul;118(1):178-89. *
Vitamin E
Tsoureli-Nikita E, Hercogova J, Lotti T, Menchini G.Evaluation of dietary intake of vitamin E in the treatment of atopic dermatitis: a study of the clinical course and evaluation of the immunoglobulin E serum levels. Int J Dermatol. 2002 Mar;41(3):146-50. *
Wiser J, Alexis NE, Jiang Q, Wu W, Robinette C, Roubey R, Peden DB. In vivo gamma-tocopherol supplementation decreases systemic oxidative stress and cytokine responses of human monocytes in normal and asthmatic subjects. Free Radic Biol Med. 2008 Jul 1;45(1):40-9. Epub 2008 Mar 12. *
Omega 3
Koch C, Dölle S, Metzger M, Rasche C, Jungclas H, Rühl R, Renz H, Worm M. Docosahexaenoic acid (DHA) supplementation in atopic eczema: a randomized, double-blind, controlled trial. Br J Dermatol. 2008 Apr;158(4):786-92. Epub 2008 Jan 30.Ashwagandha
Malik F, Singh J, Khajuria A, Suri KA, Satti NK, Singh S, Kaul MK, Kumar A, Bhatia A, Qazi GN. A standardized root extract of Withania somnifera and its major constituent withanolide-A elicit humoral and cell-mediated immuneresponses by up regulation of Th1-dominant polarization in BALB/c mice. Life Sci. 2007 Mar 27;80(16):1525-38. Epub 2007 Jan 25. *
Edited by Wulf, 02 August 2008 - 11:10 AM.