http://www.nytimes.c...nce/24stem.html
http://www.nytimes.c...nce/24stem.html In the beginning there are the stem cells: They stand ready to grow into what the body requires, and one day scientists may be able to design them to cure diseases or disability. Above, in a lab dish, cells derived from an embryo are developing into two different types of brain cells, neurons (red) and glia (green). Stem Cells: Promise, in Search of Results
In the beginning there are the stem cells: They stand ready to grow into what the body requires, and one day scientists may be able to design them to cure diseases or disability. Above, in a lab dish, cells derived from an embryo are developing into two different types of brain cells, neurons (red) and glia (green). Stem Cells: Promise, in Search of ResultsBy GINA KOLATA
Published: August 24, 2004
BOSTON - At three laboratories here, separated by a taxi ride of no more than 10 or 15 minutes, the world of stem cell research can be captured in all its complexity, promise and diversity.
One of the labs focuses on cells taken from human embryos, another on cells from mice and fish, and a third from stem cells that have mysteriously survived in the adult body long after their original mission is over.
But while the work here and elsewhere has touched off a debate reaching into the presidential campaign, a tour through these labs shows that the progress of research is both greater and less than it seems from a distance.
One idea, the focus of about half the nation's stem cell research, involves studying stem cells that are naturally present in adults. Researchers have found such cells in a variety of tissues and organs and say they seem to be a part of the body's normal repair mechanism. There are no ethical issues in studying these cells, but the problem is in putting them to work to treat diseases. So far, no one has succeeded.
The other line of research, with stem cells from embryos, has a different obstacle. Although, in theory, the cells could be coaxed into developing into any of the body's specialized cells, so far scientists are still working on ways to direct their growth in the laboratory and they have not yet effectively cured diseases, even in animals.
The most progress with embryonic stem cells is in mice, where one group of researchers directed the cells to grow into a variety of blood cells, but not yet the ones they want. Another group directed mouse stem cells to grow into nerve cells and tried to use them to treat Parkinson's disease in mice. The nerve cells produced the missing chemical, dopamine, but not enough to cure the disease.
As the two lines of research proceed along parallel paths, researchers say it is far too soon to bet on which, if either, will yield cures first. "It's not either-or," said Dr. Diana Bianchi, chief of the division of medical genetics at Tufts New England Medical Center in Boston.
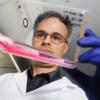
 Robert Spencer for The New York Times
Robert Spencer for The New York Times
Dr. Diana Bianchi discovered that fetal cells remain in a woman's body for decades after pregnancy, perhaps indefinitely. At the medical center, Dr. Bianchi says, her foray into the world of stem cell research involved a decade of discoveries so unexpected that despite her stellar reputation, colleagues at first looked askance.
Dr. Bianchi, who works in a lab stretched out along a narrow corridor of an old building that was once a garment factory, stumbled into the field when she was trying to find a new method of prenatal diagnosis.
She knew that a few fetal cells enter a woman's blood during pregnancy and hoped to extract those cells for prenatal diagnosis. That proved too difficult because there are so few fetal cells in maternal blood.
But then she discovered that the fetal cells do not disappear when a pregnancy ends. Instead, they remain in a woman's body for decades, perhaps indefinitely. And if a woman's tissues or organs are injured, fetal cells from her baby migrate there, divide and turn into the needed cell type, be it thyroid or liver, intestine or gallbladder, cervix or spleen.
She and her colleagues find fetal cells by looking for male cells in tissues and organs of women who have been pregnant with boys and showing that the cells' DNA matches that of the women's sons or, if the women had abortions, their male fetuses. (Cells from female fetuses also enter a woman's body, but it is quicker and easier to find the male cells by looking for cells with a Y chromosome, Dr. Bianchi says.)
One woman, for example had hepatitis C, a viral infection. But when her liver repaired itself, it used cells that were not her own.
"Her entire liver was repopulated with male cells," Dr. Bianchi said.
Such findings astonished even Dr. Bianchi. But now, with publications in leading journals, including, last month, The Journal of the American Medical Association, few doubt her.
In theory, fetal cells lurking in a woman's body are the equivalent of a new source of stem cells and could be stimulated to treat diseases. But, Dr. Bianchi says, she does not yet know for sure that the cells are stem cells - she must isolate them and prove they can turn into any of the body's specialized cells - nor where the cells reside, or how, short of injury, to spur them to action.
Using Mice and Fish, for NowA short distance away, Dr. Leonard Zon, the chief of stem cell research at Children's Hospital, and his colleague Dr. George Q. Daley are working with stem cells from embryos, using mice and zebra fish for now. They want to learn how to transform the stem cells into immature blood cells that will divide and replenish themselves.
Then, if they can apply their work to human embryonic stem cells, they want to use the cells instead of bone marrow transplants to treat patients with genetic disorders like sickle cell anemia, and inborn disorders of the immune system.
Dr. Zon treats children with these diseases, most of whom do not have a relative whose cells match theirs closely enough to serve as a bone marrow donor. He urgently wants to help.
But he is not there yet. So far, in research that stem cell investigators say is among the most promising in the field, Dr. Zon and Dr. Daley have turned mouse embryonic stem cells into mouse blood cells. Those blood cells, however, are more mature than the ones they need, a particular type of early blood cells that can repopulate a patient's bone marrow and survive indefinitely. Ones that are more mature live out their lifespans and die within weeks.
They are also working with human embryonic stem cells, venturing into the most controversial area of stem cell work. Human embryonic stem cells are derived from human embryos, about a week old, and the only way to get the stem cells is to destroy the embryos.
Some human stem cells came from embryos that were donated by couples at fertility labs who had embryos left over after they decided their families were complete. Others came from embryos that were created to obtain stem cells; researchers paid women to donate eggs, fertilized them and let them grow to the stage where stem cells could be extracted.
The federal government has agreed to pay for research with human stem cells, but only for work with 22 lines; each line is the progeny of a single embryo. That restriction dates from Aug. 9, 2001, when President Bush issued a directive saying the government would pay for research, but only with cell lines created before that date.
Dr. James F. Battey, director of the National Institute on Deafness and Other Communication Disorders and chairman of the National Institute of Health's stem cell task force, said scientists were free to study other stem cell lines if they used private money. He understands the researchers' complaints that it would be better if the government paid for work on more lines, but, he said, as far as the federal government is concerned, "the argument isn't solely about science."
"What the president has already said on multiple occasions is that he is committed to the notion that taxpayers' money should not be used to encourage the destruction of human embryos," Dr. Battey said. "This is a White House policy."
And, he said, "it is not based solely on the needs of the scientific community."
But Dr. Zon said being able to work on more human stem cell lines could help the research.
"When you are trying to do research, you look for every advantage you can," he said. "Some embryonic stem cell lines make particular tissues better than others."
Some, for example, might more easily turn into blood cells, and others might more easily grow into nerve cells, but there is no way to know whether there is a better stem cell line for a particular cell type without trying as many as possible, Dr. Zon said. "You would want to find the line that makes the tissue you are studying."
An Embryo by CloningAcross the river in Cambridge, in the basement of a biology building on Harvard's campus, a small group of scientists works in a two-room lab on the site of a former machine shop. Among their goals is to plunge into one of the most controversial areas of stem cell research - creating human embryos by cloning and obtaining stem cells from those embryos.
An embryo created by cloning would be an exact genetic match of the person whose cells were used to make it. Its stem cells and any mature cells derived from those stem cells would exactly match the cells in the person's body, making them perfect replacement cells.
One of the four part-time researchers at the Harvard lab, Dr. Kevin Eggan, learned to clone mice as a Ph.D. student at M.I.T. and, he said, the group is seeking approval from Harvard's ethics committee to try to start the cloning process with human cells.
The federal government forbids the use of its money to pay for such research, but this lab, directed by Dr. Douglas A. Melton, a Harvard developmental biologist, takes no federal money. Instead, the work is paid for by the Howard Hughes Foundation, the Juvenile Diabetes Foundation and the Naomi Berry Diabetes Center of Columbia University.
Cloning, however, can be onerous. In February, researchers in South Korea announced that they gotten stem cells from human embryos they created by cloning, but they began with 176 human eggs and ended up with one embryo that yielded stem cells.
Dr. Eggan, though, is not after replacement cells. His goal in cloning is to understand what goes wrong in a disease like Alzheimer's, Parkinson's or diabetes.
Dr. Melton gave an example. Suppose he had stem cells that were exact matches of 50 patients with Parkinson's disease and directed them to grow in the laboratory into nerve cells of the type that die in the disease. He could then ask when, and why, the cells die.
"Do they all show a defect at the same stage? If so, that would mean there is a common cause, like a flat tire. Or maybe each one breaks down in a different way. Is there one way to get Parkinson's, or 50 ways?" Dr. Melton asked.
"We could use that information to do drug screening," he added, possibly finding ways to prevent the nerve cell death.
For now, though, the Harvard lab is becoming a supplier to the world of its own 17 lines of human embryonic stem cells, created without cloning, and made from 286 frozen embryos created by in vitro fertilization.
Realism About TreatmentsMeanwhile the national debate over the use of human embryonic stem cells goes on.
While many Americans say in polls that they favor using these cells, many others have strong moral objections. Creating and destroying a human embryo to obtain stem cells, they say, is ethically unacceptable, and doing research on human embryonic stem cell lines that are already in existence does not right the wrong.
It is "a kind of after-the-fact cooperation with this destruction," said Richard Doerflinger, deputy director of pro-life activities for the United States Conference of Catholic Bishops.
The challenge for scientists in the midst of a fierce political debate, many say, is to be realistic about how hard it is to develop treatments.
Dr. Battey lists some of the challenges ahead: getting the cells to develop into exactly the adult cells that are needed, demonstrating that the adult cells can survive, preventing rejection and controlling cell growth.
Such issues, Dr. Battey said, "need to be addressed in animal models before any thoughtful person would go into humans."