The Mills study, http://www.cell.com/...6)30495-8.pdf, showed that NMN raised NAD+ levels in the liver, skeletal muscle and cortex.
It also does in this study, the debate is about the mechanism

Posted 22 March 2018 - 03:02 PM
The Mills study, http://www.cell.com/...6)30495-8.pdf, showed that NMN raised NAD+ levels in the liver, skeletal muscle and cortex.
It also does in this study, the debate is about the mechanism
Posted 22 March 2018 - 03:45 PM
Stefan.
Why do you say "For NMN I find it peculiar that even with IV it doesnt get to circulation."
When from the Liu Abstract.
"We also showed that intravenous, but not oral administration of NR or NMN delivered intact molecules to multiple tissues."
please have a look at the attached graph (2.7 figure)
Yes, clearly at this small dosage NMN doesn't REMAIN in circulation. But clearly it also GETS to circulation, hence it's rapid appearance in tissues throughout the body.
We had this discussion before. After 5 minutes all NMN is gone but only in the kidney NAD is up. Where is the NMN? Floating around as NR and NAM?
Or blood NAD+. Since NMN is the closest to NAD+, this tiny dosage could be converted to NAD+ in blood (and a little in kidney ) too quickly to register as NMN.
A small amount appears to be degraded back to NR.
I agree it does seem strange that NO NMN is found after injection, contrary to numerous prior studies. Either their detection is faulty, or, the tiny dose is utilized too quickly.
Edited by able, 22 March 2018 - 03:49 PM.
Posted 26 March 2018 - 07:34 PM
At this point, based on three studies in which NR and NMN have been directly compared, it appears that — at least in mice! — NR is the slightly superior NAD+ precursor. It's conceivable that NMN may have some advantages not captured by these studies (particularly as regards extracellular NAMPT and the hypothalamus, which I won't address here), but these studies seem consistent and are done by three independent groups.
Acute Dosing Studies
Amidst the extensive arguments on the relative advantages of NR vs. NMN leading up to and throughout the discussion of the Liu thesis, people seem to be ignoring or unaware of the the Ratajczak paper, PMID 27725675, about which both I and Ron H have posted (thank you, Ron, for that excellent and well-researched dive!). It provides some of the strongest evidence to date on this point: a direct, head-to-head test of the effect of both of these supplements on tissue NAD+ levels and other aspects of the NAD+ metabolome. Plus, it also compares them both with NAM, which (being cheap and readily-available, and not clearly risking diabetes unlike NA) is a highly salient comparator, and it measures both absolute levels and relative increases, rather than partitioning as in the Liu thesis. It also is useful as a way to compare what NAM alone would do in a tissue to what a supplement that can be metabolized into NAM does.

Figure 7, Ratajczak et al, Nat Commun. 2016 Oct 11;7:13103 (PMID 27725675)
In looking at this Figure, you'll want to first look just at the white bars, which are for wild-type mice — and particularly the data on the left (ie, (a), ©, (e), and (g)), which are for absolute NAD+ levels (whereas the graphs on the right (b, d, f, and h) show the relative increase in NAD+ after supplementation, relative to baseline levels). Here we see pretty clearly that NR is —in these animals — a very slightly better NAD+ precursor than NMN (most clearly in the liver), and both are somewhat better precursors than NAM (particularly in the kidney).
Then, compare the values in the white bars for a given supplement to the black bars. Whereas the white bars give you the effect of a given supplement on tissue NAD+ in wild-type mice, the black bars have data for animals with NRK1 knocked out, so they can't transport NR into their tissues. The fact that the white bars are consistently a bit higher than the black bars is quite strong evidence that the increase in NAD+ in peripheral tissues is not just due to NAM produced secondary to NR or NMN metabolism in the liver: if it were, then they wouldn't need NRK1 to get their NAD+ levels raised, because it would be done in all cases by NAM, which doesn't rely on NRK1 for transport. Along with other evidence in the paper) pretty darned convincing evidence that while the majority of the elevation in NAD+ delivered by NR or NMN comes via secondary metabolism or degradation to NAM and back into NAD+ via NAMPT, rather than directly from either one, some actual NR or NMN must also be directly reaching the tissue and contributing to the boost. Note that no such effect is seen for NAM. Additionally, they show that NMN does indeed need to be converted into NR in order to be used to make NAD+ (presumably extracellularly, by CD73), as otherwise there would again be no effect of NRK1.
But granted that we all presumably have intact NRK1, the most relevant data for present purposes are the white bars.
Some things to bear in mind about this study. First, while it's not totally clear, it appears that all mice were likely C57BL/6NTac — a strain that, unlike the C57BL/6J mice used in nearly all other NR and NMN studies, does not bear the NNT mutation. It's not clear because they don't say: the NRK1-KO mice are specifically said to be on a C57BL/6NTac background, whereas AFAICS the strain of the "wild-type" mice is never specified. It would certainly be best if they had used the same strain for both, both because you want to be comparing apples and apples, and because humans have an intact NNT gene. How much this should matter for simple NAD+ levels (as opposed to the benefit from raising such levels) is not clear, especially in a short-term study like this: what you primarily predict is a difference in NAD+:NADH and especially NADP+:NADPH, and also differences in redox tone, metabolism, and (most importantly) health and functional outcomes — none of which are measured in this paper. IAC, a strain of mouse that does not have the NNT mutation is likely to be more valid for normal human translation.
Second, note that they administered the supplements via intraperitoneal injection, rather than orally. This is unfortunate, as we'd really want to see as close as possible to human supplementation; however, i.p. injection shouldn't make too much of a difference in this case (unlike for things that are biotransformed in the intestines or subject to extensive enterohepatic circulation), because the primary route of absorption after i.p injection is via the mesenteric vessels, which drain into the portal vein and pass through the liver, thereby undergoing hepatic metabolism before reaching the systemic circulation. This is important because of the evidence (reinforced here) that a lot of the direct effects of NR or NMN on NAD+ occur in the liver before they (and, importantly, NAM derived from their metabolism) is secondarily released into the circulation: intravenous injection would bypass this, potentially exaggerating the effects of these supplements over NAM in distant tissues.The only real worry here is possible degradation or metabolism in the intestinal tract itself (repeatedly raised by Turnbuckle), and this should be no less of a worry (and maybe a little more) for NMN than for NR, so NR's advantage here can't reasonably be discounted on that basis.
Third, note that they used 500 mg/kg of each precursor in the above graph. That's "milligrams per kg" — unlike Trammel & Brenner PMID 27721479, which compared 185 mg/kg NR to the mole equivalent doses of NAM and NA. That may have been a scientifically justifiable thing to do, but if you're shopping for supplements, it may be more relevant to compare them on a mg-for-mg basis. As has been loudly pointed out previously, 185 mg/kg NR (molecular weight 255.2472 g/mol — or, for NRCl, 290.7 g/mol) is equivalent on an isomolar basis to 77.7 mg/kg NAM (MW 122.12 g/mol), 78.35 mg/kg NA (MW 123.11 g/mol), or (tho' they didn't compare it) 212.7 mg/kg NMN (MW 334.221 g/mol). So in terms most relevant to a "supplement user on the street," Trammel & Brenner were declaring NR to be an "uniquely bioavailable" NAD+ precursor after more or less comparing a given dose of NR to only half as much NAM or NA. Here, instead, they were using the same number of milligrams of each supplement.
Note also that 500 mg/kg is in line with the doses used in most of the rodent studies with actual health outcomes. However, it's also much higher than is reasonable for anyone to take (on cost, caution, safety (GRAS paper, production of N-methylnicotinamide, redox imbalance) and likely ceiling effects and homeostatic counterregulatory responses (see most especially the Elysium trial): depending on your assumptions, somewhere in the 2000 to 4000 mg doses for a 70 kg human. It's also reasonable to assume that the pharmacodynamics would be different at a lower dose — most likely, in the direction of leveling down the differences rather than enhancing them.
Happily, they did partially address this with their studies presented in Supplementary Figure 3, using only 50 mg/kg in the liver (left)— same as in the Liu thesis, and more in line with realistic human dosing (50 mg/kg in a likely 25 g mouse ≈ 284 mg in a 70 kg human per FDA HED, or 481 mg per direct allometric scaling). Note, however, that these are all percentage increases, and that the muscle values on the right are again at 500 mg/kg:
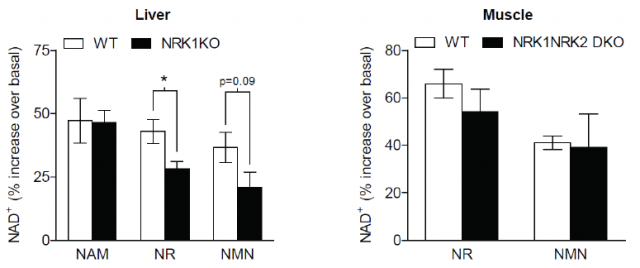
Supplementary Figure 3, Ratajczak et al, Nat Commun. 2016 Oct 11;7:13103 (PMID 27725675)
Note that at this lower dose, NAM is actually as good as NR at raising NAD+ in the liver. That's arguably consistent with Trammel & Brenner PMID 27721479, which used doses closer to this lower level,especially considering that T&B used twice as much NR as NAM on a milligram basis: 185 mg/kg NR vs. 77.7 mg/kg NAM. However, we also know from Trammel & Brenner that NAM raises 1N-methylnicotinamide dramatically more than NR even when given at half the dose of NR in their study. Additionally, in the NAM lifespan study, long-term NAM use actually didn't sustain high NAD+ levels long-term — more on this below. So, to anticipate: between those consideration and the clear advantage of NR (and less so, NMN) over NAM in other tissues at higher doses, I don't think this justifies preferring NAM over the "novel" precursors.
And, finally, there is Frederick & Baur PMID 27508874. They used mice with NAMPT knocked out in their muscle cells only : thus, while they could use NAM to make NAD+ in their livers and most other tissues, they were unable to use NAM to synthesize NMN (and thence NAD+) directly in their muscles. Here they not only find, somewhat contrary to other studies, that NR raises liver NAD+ much more than NAM in these mice;and that — consistent with others — most NR does first get converted to NAD+ in the liver and metabolized via SIRTs and PARPs and others into NAM, which is then released into the plasma: "[O]ral NR dosing increased circulating NAM ≈40-fold, while NMN remained unchanged and NR was detected only at trace levels in the blood. Thus, the majority of the orally administered NR that reaches the muscle appears to enter in the form of liberated NAM or as NMN (Figures 6G and 6H)."
But despite this, they find that NR raises NAD+ significantly more in the muscle than does NAM (Supplemental Fig. 5I):

Frederick & Baur, Cell Metab. 2016 Aug 9;24(2):269-82. PMID: 27508874.
But again, these mice can't use NAM to make NAD+ in their muscles, whether that's NAM coming directly from NAM supplements or NAM derived from NR metabolism in the liver. So either that small residual level of serum NR is being used to make a surprising amount of NAD+ in the muscle, or there's some other indirect mechanism — or Frederick & Baur just had a hard time detecting NR in serum, which we know to be a problem, and circulating levels were actually significantly higher than the trace levels they detect. Ratajczak and others speculate that part of the problem is that most studies measure circulating NR in plasma, whereas they note that "NR is stably associated with protein fractions in milk with a lifetime of weeks and [they speculate] may be circulated in a cell-associated form in animals with a lifetime of hours." In fact, we know this to be true in humans after oral administration, thanks to the UWash pharmacodynamic study, which clearly shows a substantial rise in whole-blood NR after oral administration, with the amount of elevation apparently loosely proportional to one's baseline levels, with a Tmax of ≈3 h and a half-life of 2.7 h.
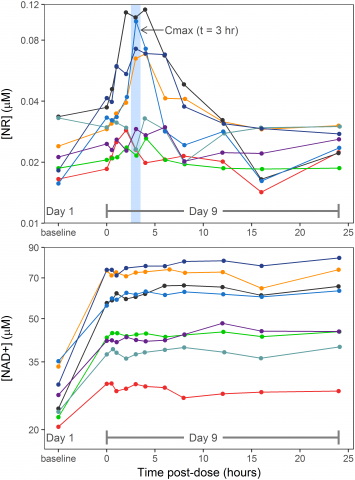
Figure 3, PLoS ONE 12(12): e0186459, PMID 29211728
Either way, advantage: NR once again.
To sum up, in all of these studies it seems reasonably clear that the level of NAD+ increase afforded by various precursors is roughly NR > NMN > NAM, with the magnitude of the effect varying by dose and tissue. One important question mark is (the adipokine-like influence of adipose tissue-derived eNAMPT on hypothalamic NAD+, and even that is most clearly influenced by adipose NAD+ and SIRT1 activity: an effect of circulating NMN or NR has been speculated — but we lack direct evidence for such an effect, and that's a subject for another day).
However, these are all from one-time dosing of naïve animals. What happens after longer-term supplementation, when metabolic adjustmnts, chronic exposures, and feedback loops set in?
Subacute Supplementation
We have here an oft-neglected data point is from one of the first NR studies to make a splash — Cantó and Auwerx PMID 22682224:

Figure 1, Cantó and Auwerx, Cell Metab. 2012 Jun 6;15(6):838-47.PubMed PMID: 22682224
This is very useful not only for providing direct comparative data, but also because it was NR administered in chow (not gavage or any kind of injection); because each supplement was given at the same mass dose (400 mg/kg); and because NAD+ levels were measured after a week of treatment, not just acutely as in Liu or the studies reviewed in the first section above. Here we see in Figure 1(d) that NR (and, notably, nicotinic acid) raise hepatic and muscle NAD+ more than isomolar NMN on a subchronic basis.
Now, again: does this mean we should favor cheap, well-studied nicotinic acid over NR or NMN? I would say not, because of the well-established risk of diabetes. We have no long-term data to go by in humans for NR or NMN, but we do at least know that the latter seem to reduce the risk of obesity- or age-related diabetes in mice, and that neither engages the suspect GPR109a receptor (Fig. 1(b) above, and discussion here).
Long-Term Sustainability
This is an even more important question, of course. The boost afforded by these precursors might well be transient, and eroded over time by metabolic adjustment and homeostatic feedback systems. There's clear evidence of this. For instance, all the data on NAM above shows that it does at least initially raise tissue NAD+ levels (even if not to the same degree as the novel precursors) — yet in the NAM lifespan study (Mitchell & de Cabo PMID 29514072), long-term NAM use actually didn't sustain high NAD+ levels long-term, at least in the liver (the only place they looked), apparently due to a profound negative feedback on NAMPT, with partial compensation via the kynurenine (tryptophan) pathway.
Similarly, in the Elysium Basis trial PMID 29184669, NR raised blood NAD+ for the first 30 days, but by day 60 there was a clear erosion of that boost at the 60-day point at 500 mg/d, and the suggestion of a similar decline at the 250 mg/d dose:
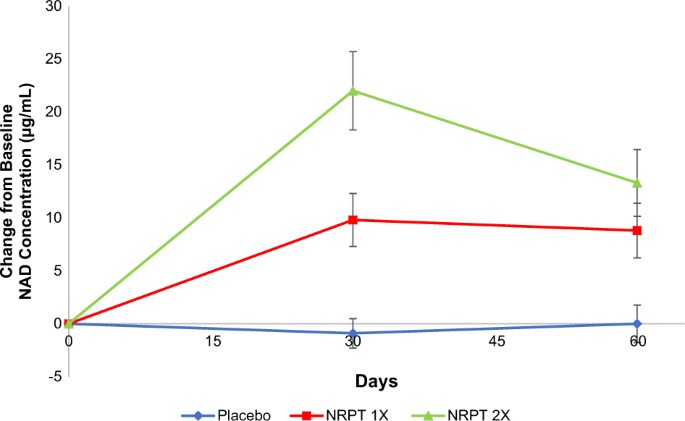
I think we also see some evidence for this in the long-term NMN study (PMID 28068222). After 6 months of NMN administration (from adulthood (5 mo) to early middle age at 11 mo) at relatively moderate doses of 100 and 300 mg/kg, NAD+ levels were higher in supplemented vs. unsupplemented animals "in the liver and BAT, but not in other tissues including skeletal muscle and WAT" — and even in those tissues, the increase in tissue NAD+ vs. age-matched controls seems pretty modest, tho' perhaps in line with what you might expect from just extrapolating the acute dosing studies (Figure 1(e):

Figure 1, Mills et al, Cell Metab. 2016 Dec 13;24(6):795-806. PMID 28068222.
Unfortunately, AFAICS, we lack equivalent long-term data for NR, but the Elysium trial already tells us that this is an issue.
OTOH, we do see from all of the long(ish)-term studies on NAD+ precursors that supplementation leads to improved health outcomes, despite the fact that NAD+ increases are either not sustained or are very modest. Even the NAM lifespan study found significant benefits for supplemented animals on a high-fat, diabesogenic diet, similar to what's been reported for NR and NMN. Frederick & Baur PMID 27508874, observing that a very modest difference in tissue NAD+ levels between NAM- and NR-supplemented anmals led to significant differences in muscle function, speculated that:
In light of its potent phenotypic effects in mNKO mice, we were surprised to find that NR exerts only a subtle influence on the steady-state concentration of NAD in muscles. Our tracer studies suggest that this is largely attributable to breakdown of orally delivered NR into NAM prior to reaching the muscle. Nonetheless, our results indicate that NR is more effective than NAM for reversing mNKO phenotypes (Figure S5). The correlation between the NAD content and the respiratory capacity of isolated mitochondria, even in cultured myotubes (Figure 4), supports the model that subtle changes in NAD can disproportionately modulate aerobic metabolism. It is important to note that NAD turnover may vary independently from NAD concentration and that small changes in average tissue concentration might reflect larger changes in specific cells or subcellular compartments. It is also possible that intramuscular conversion of NAD into secondary messengers potently influences calcium homeostasis, which is both essential to muscle contraction and can independently modulate mitochondrial respiration (Cárdenas et al., 2010).
Our results leave open the possibility that some of the functional improvements in NR-treated mNKO muscles are secondary to effects in other cell types. Because necrosis was decreased by both NR and NAM at the time point examined in our study, the net effect on the regenerative capacity of satellite cells is not clear and will be an important focus of future work. The observation that NAM treatment was sufficient to confer a partial effect in mNKO muscle supports the model that effects outside of differentiated fibers contribute to the benefits of NR. Such indirect activities may help to explain how oral NR administration clearly mitigates the severity of insults to a growing list of tissues in which robust NAD decrements were not observed before treatment (Brown et al., 2014; Cerutti et al., 2014; Khan et al., 2014; Xu et al., 2015). We also cannot exclude the possibility that NAM contributes slightly to the NAD pool in mNKO myofibers by inhibition of NAM-sensitive NAD consumers or via residual Nampt activity in fibers or fusing myoblasts.
But if the benefits of precursor supplementation are due to subtle non-NAD+-related effects of subcellular distribution, you clearly can't just look at effects on NAD+ levels (especially in short-term studies) and use them as a surrogate for health benefits.
Addressing some of Ron's very valuable notes:
First, there is the matter of stability of NR vs NMN in serum.
According to Ratajczak's data, some 66% of NR incubated in serum disappears in 1 hour, whereas NMN is stable under these conditions. The observation that NR is partially converted into Nam does not tell me much: if you compare the counts in their Figs 8e and 8g, you can see that only some 5% of NR is converted into Nam. This may still be a lot under their experimental conditions (high doses and short incubation times, and suggested by their supplementary Fig. 4c), but I wonder how this translates to humans taking low doses of NMN or NR once or twice daily.
Well, you're basing that on data in mouse plasma, whereas (as mentioned above) they note that "NR is stably associated with protein fractions in milk with a lifetime of weeks and [they speculate] may be circulated in a cell-associated form in animals with a lifetime of hours." In fact, we know this to be true in humans after oral administration, thanks to the UWash pharmacodynamic study, which clearly shows a substantial rise in whole-blood NR after oral administration (above).
I could make the case that oral NMN is stable in plasma and that orally ingested NMN will lead to levels of circulating NMN that are much higher than the levels of circulating NR in the case of equimolar orally ingested NR. ...
Ratajczak's suggestion that NR may be circulating in a cell-associated form in animals with a lifetime of hours may be correct and thus change the picture, but at present this is not backed by any direct experimental data.
As the UWash authors note, Ratajczak et al's guess appears to be correct: after a blood draw, NR is indeed unstable in blood and indetectable in plasma ex vivo, yet with rapid processing they can detect it (and, importantly, the post-dose rise) in whole blood when processed rapidly. "We concluded that NR is concentrated in the cellular fraction of blood."
This is, IAC, somewhat of a side issue. We aren't ultimately concerned with the level of NR, NMN, or any other NAD+ precursor in plasma or blood, but the effect of supplementation on tissue NAD+. From a tissue NAD+ perspective, the differences appear to be modest, but advantage: NR.
However:
Second, there is the matter of CD73.
A general line of reasoning, at least by people posting in this forum, is that NR is better than NMN at boosting NAD+ synthesis, simply because NMN needs to be converted by CD73 to NR before it can enter the cell, whereas NR itself enters the cell directly. In fact, this seems to be corroborated by most head-to-head comparisons of NR and NMN in the Ratajczak paper. Such comparisons are shown in Figs 2d and e, 4, 5e, 6a (controls), 7 and 8a.
However, there are a few caveats here:Taken together, I think that the conclusion that NR is better than NMN at boosting NAD+ synthesis is only true when dealing with very high NR concentrations and low CD73 levels. I find it premature to conclude that NR would be better than NMN at raising tissue NAD+ levels in humans taking low doses of NR or NMN.
- First, it should be kept in mind that in Figs 1-7 very high NR concentrations are used and that therefore the cells' equilibrative nucleoside transporters (ENTs) may be saturated. This would mask any advantage that a local increase in NR concentration through NMN dephosphorylation by CD73 might have.
- The cell lines used in Figures 2 and 4 have low levels of CD73:
- In Figure 2 3T3 cells are used. Apparently, only some 3% of NIH/3T3 cells express CD73 (see Fig. 3 of ref. 1)
- In Figure 4 HepG2 cells are used. In human liver, alternative splicing of the NTE5E gene (encoding CD73) leads to two transcripts: NT5E-1 encoding functional CD73, and NT5E-2 encoding an inactive form of CD73 that lacks 5′-nucleotidase activity and that promotes degradation of active CD732. Relative to the normal human liver, the expression levels of the NT5E-2 transcript are increased by one to two orders of magnitude in the HepG2 cell line, whereas NT5E-1 levels are decreased (see Fig. 3 of ref. 2).
- In Figs 5 and 6 hepatocytes from WT or NRK1KO mice are used, but the cells were grown under serum-free conditions. Again, the absence of serum and concomitant very high NR concentrations might mask any advantage that a local increase in NR concentration through NMN dephosphorylation by CD73 might have.
- In Figs 7 and 8 whole animals are used. The mouse strain used in this study is a derivative of the C57BL strain and, for what it's worth, in a comparative study the livers of C57BL mice were shown to contain significantly less CD73 protein- and mRNA levels than another strain3. Nevertheless, I find it striking that in Figure 7 of the Ratajczak paper only in kidney the effects of NR and NMN are indistinguishable, and that CD73 levels in this organ are clearly higher than in the other tissues (cf. their supplementary Fig. 3a). In Figure 8 10-fold lower doses of NR and NMN are used and here the advantage of NR over NMN disappears.
Yeah, this is very cogent — thanks. I note that human CD73 expression seems uniformly high at the protein level, except in adipose. OTOH:
•Even in kidney, NAD+ levels after NMN administration are only equivalent to those after NR, not superior (tho' there's a hint of superiority in the Liu paper);
• The full text of the report finding reduced CD73 protein- and mRNA levels in livers of "C57BL mice" than in C3H/He indicates that the "C57BL mice" were, in fact, "C57Bl/6J; these diverged from the 6N strains back in the 1940s or 50s, and in addition to the prominent NNT mutation, have a fair number of other genetic differences from the 6N substrains (which also have differences in sub-substrains, but tend to be more uniform to each other than the 6J strains are to each other). I did a pretty extensive dig, and to my frustration couldn't find any data on CD73 expression in 6N, unfortunately.
• These are, of course, very tentative arguments and speculations, based on tissue transporter expression levels and very slight reported differences at different doses. We'd all like to see studies in more animals (especially Homo sapiens), over a wider range of doses, and for longer time-periods with multiple samples, but the data to hand does seem to rather consistently favor NR.
Posted 26 March 2018 - 08:27 PM
Posted 26 March 2018 - 08:57 PM
Posted 26 March 2018 - 09:25 PM
@Michael, wow that is a paper in itself. Going to read that in peace. Thank you.
Posted 26 March 2018 - 10:44 PM
AGREED!
Posted 27 March 2018 - 12:43 AM
Posted 27 March 2018 - 01:35 AM
This seems like resveratrol part 2. I don't see anyone reverse aging except Sinclair's mice for which another study just came out and no one here seems to even know.
Wake me up when injectible NMN is available and affordable.
Until then I will keep alternating liposomal resveratrol with niacin. With niacin i can see it in my blood work... Can anyone here see NR in their bloodwork? I here a few anecdotes without data.
Show me the data you are reverse aging like Sinclair's mice!
Posted 27 March 2018 - 12:27 PM
This seems like resveratrol part 2. I don't see anyone reverse aging except Sinclair's mice for which another study just came out and no one here seems to even know.
Wake me up when injectible NMN is available and affordable.
Until then I will keep alternating liposomal resveratrol with niacin. With niacin i can see it in my blood work... Can anyone here see NR in their bloodwork? I here a few anecdotes without data.
Show me the data you are reverse aging like Sinclair's mice!
Where have you been? A large of proportion of people taking NR saw anti aging effects. Most people can see the benefits in blood work such as reduced LDL and triglycerides and improved kidney function. People who have been on Niacin for many years saw big improvements in health after taking NR. I agree that bioavailability studies in mice are not demonstrating NR and NMN to be much better than NAM, but clinical data shows otherwise.
This response is to Rocket, just picked the wrong one to quote.
I tried to get others to post their blood test results - only MikeDC and I have said anything about them so far as I know, but the personal experiences thread may have some postings on it (it is long and I'm not digging through that today for you).
Anyway, here are mine:
http://www.longecity...64-blood-tests/
My primary care physician had a hemotologist look at the WBC and RBC as I was somewhat concerned about that and that doctor said it was no problem whatsoever. It was the same while on NR as when I abstained from NR, and then later after the hemotologist looked at it a third blood test showed that it came back up a little bit into the normal range somewhat. I rarely get sick anyway - like maybe once every couple years, not sure and have no problem hiking up mountains or running through the parks around my house so I suppose the hematologist was probably correct to begin with.
I think to show "Anti-Aging" in humans, we are going to have to wait several decades and then compare blood work and biomarkers of inflamation and that sort of thing, so Rocket I think you're a bit premature with the question, but definitely come back in thirty years or so and ask again.
Edited by TMNMK, 27 March 2018 - 12:38 PM.
Posted 28 March 2018 - 09:55 AM
"Low" WBC is a known effect of CR, and may be sign of beneficial reduction in ongoing inflammatory processes. "Normal" (higher WBC) #s may be unhealthy, relatively.
Edited by tintinet, 28 March 2018 - 09:56 AM.
Posted 28 March 2018 - 11:30 AM
"Low" WBC is a known effect of CR, and may be sign of beneficial reduction in ongoing inflammatory processes. "Normal" (higher WBC) #s may be unhealthy, relatively.
That's interesting, I did not know that! Thanks tintinet, I'll look that up further.
Edited by TMNMK, 28 March 2018 - 11:31 AM.
Posted 28 March 2018 - 08:07 PM
At this point, based on three studies in which NR and NMN have been directly compared, it appears that — at least in mice! — NR is the slightly superior NAD+ precursor.
Figure 3, PLoS ONE 12(12): e0186459, PMID 29211728
long-term NMN study (PMID 28068222). (Figure 1(e):
Figure 1, Mills et al, Cell Metab. 2016 Dec 13;24(6):795-806. PMID 28068222.
... the data to hand does seem to rather consistently favor NR.
Not sure it's a fair conclusion to favor oral ingestion of NR over NMN, particularly in view of the above Day 1 comparative charts from the 2 studies above. Especially considering that NR, NMN, and NAD+ are thought to cycle states among one another inside the body after ingestion suggesting limited significance in blood levels of only 1 or 2 of them without measuring any others. See: https://www.ncbi.nlm...pubmed/29249689

Notice for instance how in the UWash study NR showed no peaking at all on day 1. Just a slow and steady increase in blood levels of NR over a 24 hour period, long after that dosage was probably gone from the digestive tract. I think that would be consistent with previous studies finding no direct NR absorption in the digestive tract with all converted to NAD+ before absorption with blood serum levels attributed to subsequent state changes. The peaking on day 9 is interesting but in light of day 1, not indicative of direct absorption. It might have been more informative if UWash had measured NR, NMN, NAD+ and perhaps eNAMPT together and compared ingestion of both NR and NMN. I hope they at least repeat it for NMN because I think the comparative day 9 NAD+ measurements would be dispositive.
In contrast the NMN study chart does show low-level peaking of NMN in the bloodstream shortly after ingestion although only for 10 minutes. This suggests some direct absorption but gives no clue if that actually goes anywhere of significance... I note that the right-hand x-axis overlay is totally misleading in suggesting those low blood levels of NMN detected are responsible for the NAD+ detection elsewhere in the body, being that no effort was made to separate NAD+ detected from directly absorbed NAD+ and NMN. Similarly this study would also be more informative if it measured all 4 levels.
I hope I'm not coming off like I'm pushing one over the other. I've only actually ever taken NR. Been doing so since one of the early group buys here. But I'm leaning towards NMN when I restock in a few months. Price permitting.
Howard
Edited by hav, 28 March 2018 - 08:34 PM.
Posted 28 March 2018 - 08:36 PM
You are both misinterpreting the chart and drawing conclusions without any reasoning. The U of W chart shows NR at baseline on day 1 increased to steady state at 0 hour on day 9. The line is not real data points. The baseline NR on day 9 at 0 hours is not due to Supplemented NR. The body maintains a level of NR that is higher than NMN as shown by Ling Liu’s Dissertation. The chart shows NR peaked at hour 5. The ling liu’s Dissertation also showed that NMN and NR are absorbed at about the same rate until 135 minutes. It would be interesting to see if NMN also peaks at 5 hours. If NMN peaks at 135 min or much earlier than 5 hours, then NR is much superior than NMN. A future study that tracks NAD+ over 6 hours will finally settle the disputes. Until then NR is still better than NMN.Not sure it's a fair conclusion to favor oral ingestion of NR over NMN, particularly in view of the above Day 1 comparative charts from the 2 studies above. Especially considering that NR, NMN, and NAD+ are thought to cycle states among one another inside the body after ingestion suggesting limited significance in blood levels of only 1 or 2 of them without measuring any others. See: https://www.ncbi.nlm...pubmed/29249689At this point, based on three studies in which NR and NMN have been directly compared, it appears that — at least in mice! — NR is the slightly superior NAD+ precursor.
Figure 3, PLoS ONE 12(12): e0186459, PMID 29211728
long-term NMN study (PMID 28068222). (Figure 1(e):
Figure 1, Mills et al, Cell Metab. 2016 Dec 13;24(6):795-806. PMID 28068222.
... the data to hand does seem to rather consistently favor NR.
Notice for instance how in the UWash study NR showed no peaking at all on day 1. Just a slow and steady increase in blood levels of NR over a 24 hour period, long after that dosage was probably gone from the digestive tract. I think that would be consistent with previous studies finding no direct NR absorption in the digestive tract with all converted to NAD+ before absorption with blood serum levels attributed to subsequent state changes. The peaking on day 9 is interesting but in light of day 1, not indicative of direct absorption. It might have been more informative if UWash had measured NR, NMN, NAD+ and perhaps eNAMPT together and compared ingestion of both NR and NMN.
In contrast the NMN study chart does show low-level peaking of NMN in the bloodstream shortly after ingestion although only for 10 minutes. This suggests some direct absorption but gives no clue if that actually goes anywhere of significance... I note that the right-hand x-axis overlay is totally misleading in suggesting those low blood levels of NMN detected are responsible for the NAD+ detection elsewhere in the body, being that no effort was made to separate NAD+ detected from directly absorbed NAD+ and NMN. Similarly this study would also be more informative if it measured all 4 levels.
I hope I'm not coming off like I'm pushing one over the other. I've only actually ever taken NR. Been doing so since one of the early group buys here. But I'm leaning towards NMN when I restock in a few months. Price permitting.
Howard
Edited by MikeDC, 28 March 2018 - 08:41 PM.
Posted 28 March 2018 - 09:16 PM
"You are both misinterpreting the chart and drawing conclusions without any reasoning." Says MikeDC (our resident Chromadex shill) who is notorious for doing both. Among MikeDC's famous claims, "NR is 6,400% better than NMN."
Edited by LawrenceW, 28 March 2018 - 09:17 PM.
Posted 28 March 2018 - 09:23 PM
"You are both misinterpreting the chart and drawing conclusions without any reasoning." Says MikeDC (our resident Chromadex shill) who is notorious for doing both. Among MikeDC's famous claims, "NR is 6,400% better than NMN."
Posted 28 March 2018 - 10:44 PM
At this point, based on three studies in which NR and NMN have been directly compared, it appears that — at least in mice! — NR is the slightly superior NAD+ precursor.
Figure 3, PLoS ONE 12(12): e0186459, PMID 29211728
long-term NMN study (PMID 28068222). (Figure 1(e):
Not sure it's a fair conclusion to favor oral ingestion of NR over NMN, particularly in view of the above Day 1 comparative charts from the 2 studies above. Especially considering that NR, NMN, and NAD+ are thought to cycle states among one another inside the body after ingestion suggesting limited significance in blood levels of only 1 or 2 of them without measuring any others. See: https://www.ncbi.nlm...pubmed/29249689
Notice for instance how in the UWash study NR showed no peaking at all on day 1. Just a slow and steady increase in blood levels of NR over a 24 hour period, long after that dosage was probably gone from the digestive tract. I think that would be consistent with previous studies finding no direct NR absorption in the digestive tract with all converted to NAD+ before absorption with blood serum levels attributed to subsequent state changes. The peaking on day 9 is interesting but in light of day 1, not indicative of direct absorption. It might have been more informative if UWash had measured NR, NMN, NAD+ and perhaps eNAMPT together and compared ingestion of both NR and NMN. I hope they at least repeat it for NMN because I think the comparative day 9 NAD+ measurements would be dispositive.
In contrast the NMN study chart does show low-level peaking of NMN in the bloodstream shortly after ingestion although only for 10 minutes. ...
I hope I'm not coming off like I'm pushing one over the other. I've only actually ever taken NR.
You certainly don't come off like you're pushing one or the other (and I trust that I don't either, tho' I've come to what I think is a pretty clear conclusion on this subject), but MikeDC is in this case correct: you are misinterpreting the UWash figure. The only data we have for Day 1 is the unsupuplemented baseline, which naturally shows no supplement effect: we then see multiple data points starting on the AM of day 9, by which point as I'd mentioned users' basline NR and NAD had already been elevated by previous usage, and that by that point a single AM supplement leads to the NR peak as observed and a jump in blood NAD+ that remains about the same for 24 hours.
In any case, we really shouldn't care much about how quickly one or the other raises levels,or whether there's a peak, but about steady-state levels after long-term supplementation (or NAD+ AUC, if (hypothetically) there were not a steady-state). It's also not clear to me why we would care particularly much about levels of NR, NMN, eNAMPT and the rest except as they may inform about tissue NAD+, — but we don't have to guess about this, since as documented from multiple studies and in multiple tissues across multiple timescales, NR pretty consistently outperforms NMN. (As noted, a possible exception is the hypothalamus, where circulating NMN or NR may elevate levels via the adipokine-like influence of adipose tissue-derived eNAMPT on hypothalamic NAD+, and even that is most clearly influenced by adipose NAD+ and SIRT1 activity: an effect of circulating NMN or NR has been speculated — but we lack direct evidence for such an effect, or comparative data on hypothalamic NAD+ levels).
Posted 29 March 2018 - 05:27 AM
...
MikeDC is in this case correct: you are misinterpreting the UWash figure. The only data we have for Day 1 is the unsupuplemented baseline, which naturally shows no supplement effect: we then see multiple data points starting on the AM of day 9, by which point as I'd mentioned users' basline NR and NAD had already been elevated by previous usage, and that by that point a single AM supplement leads to the NR peak as observed and a jump in blood NAD+ that remains about the same for 24 hours.
In any case, we really shouldn't care much about how quickly one or the other raises levels,or whether there's a peak, but about steady-state levels after long-term supplementation (or NAD+ AUC, if (hypothetically) there were not a steady-state). It's also not clear to me why we would care particularly much about levels of NR, NMN, eNAMPT and the rest except as they may inform about tissue NAD+, — but we don't have to guess about this, since as documented from multiple studies and in multiple tissues across multiple timescales, NR pretty consistently outperforms NMN. (As noted, a possible exception is the hypothalamus, where circulating NMN or NR may elevate levels via the adipokine-like influence of adipose tissue-derived eNAMPT on hypothalamic NAD+, and even that is most clearly influenced by adipose NAD+ and SIRT1 activity: an effect of circulating NMN or NR has been speculated — but we lack direct evidence for such an effect, or comparative data on hypothalamic NAD+ levels).
I think you and MikeDC are right about lack of data throughout day 1... just looked more closely about what they said about that in the write-up:
Blood samples were obtained to monitor for potential side effects of NR therapy following 6-hour fasts and prior to NR dosing at baseline (Day 1) and on Days 2 and 9.
...
NR and NAD+ concentrations were determined in blood samples drawn on Day 1 as well as in samples obtained on Day 9 at the following times after the last 1000 mg NR dose: 0.5, 1, 2, 3, 4, 6, 8, 12, 16, and 24 hours
But this does not change the unfairness of drawing conclusions about nr direct absorption or comparative bioavailability of nr and nmn based on this. Inferring too much from nr detection in the bloodstream is unfounded when we know that nr, nmn, and nad+ change states from one to the other spontaneously. A more complete snapshot would help. Uncertainty on the absorption mechanism is mentioned in the report itself when commenting on the wide variations in NAD+ observed among the 8 participants:
The current study demonstrates that the apparent oral bioavailability of a 1000 mg dose of NR was highly variable among individuals. While half of the participants showed a significant increase (≥ 100%) in peak blood NR concentration during the pharmacokinetic portion of the study, the remaining subjects showed no or only modest (≤ +50%) changes in blood NR levels. The explanation for this inter-subject variability in post-dose NR levels is not obvious. The instability of NR in blood samples observed here as well as in prior studies [19] could be one contributing factor, although it cannot account for all the variability given the steps we have taken in minimizing instability during handling and processing of blood samples. Another possibility is that, based on its hydrophilicity (XLogP3 = –1.8) [20], NR is expected to exhibit low passive permeability across the human intestinal mucosa. Oral absorption of NR may rely on an active, mediated transport process that varies in active between individuals. It is also possible that NR is degraded to nicotinamide in the gut; nicotinamide is then absorbed and converted to NMN, which can further be converted to NAD+ or dephosphorylated to NR. If true, the degradation of NR to nicotinamide in the gut, which presumably involves purine nucleoside phosphorylase in mammalian and bacterial cells [21] may be a variable step involved in the oral intake of NR. Hence, investigation into the mechanism(s) of NR absorption and metabolism may afford insights into its variable oral bioavailability.
This rat study, btw, suggests their last speculation is closer to the correct one. The significance of this is that if nr is not directly absorbed, then bioavailability cannot be determined by simple bloodstream measurements and AUC calculations on nr alone. I agree that comparing resulting nad+ steady-state measurements following similar nr and nmn dosing regimens may be a more significant metric. I just don't think we have enough comparable data on that yet to choose which is more optimal.
Howard
Posted 29 March 2018 - 10:44 AM
...
MikeDC is in this case correct: you are misinterpreting the UWash figure. The only data we have for Day 1 is the unsupuplemented baseline, which naturally shows no supplement effect: we then see multiple data points starting on the AM of day 9, by which point as I'd mentioned users' basline NR and NAD had already been elevated by previous usage, and that by that point a single AM supplement leads to the NR peak as observed and a jump in blood NAD+ that remains about the same for 24 hours.
In any case, we really shouldn't care much about how quickly one or the other raises levels,or whether there's a peak, but about steady-state levels after long-term supplementation (or NAD+ AUC, if (hypothetically) there were not a steady-state). It's also not clear to me why we would care particularly much about levels of NR, NMN, eNAMPT and the rest except as they may inform about tissue NAD+, — but we don't have to guess about this, since as documented from multiple studies and in multiple tissues across multiple timescales, NR pretty consistently outperforms NMN. (As noted, a possible exception is the hypothalamus, where circulating NMN or NR may elevate levels via the adipokine-like influence of adipose tissue-derived eNAMPT on hypothalamic NAD+, and even that is most clearly influenced by adipose NAD+ and SIRT1 activity: an effect of circulating NMN or NR has been speculated — but we lack direct evidence for such an effect, or comparative data on hypothalamic NAD+ levels).
I think you and MikeDC are right about lack of data throughout day 1... just looked more closely about what they said about that in the write-up:
Blood samples were obtained to monitor for potential side effects of NR therapy following 6-hour fasts and prior to NR dosing at baseline (Day 1) and on Days 2 and 9.
...
NR and NAD+ concentrations were determined in blood samples drawn on Day 1 as well as in samples obtained on Day 9 at the following times after the last 1000 mg NR dose: 0.5, 1, 2, 3, 4, 6, 8, 12, 16, and 24 hours
But this does not change the unfairness of drawing conclusions about nr direct absorption or comparative bioavailability of nr and nmn based on this. Inferring too much from nr detection in the bloodstream is unfounded when we know that nr, nmn, and nad+ change states from one to the other spontaneously. A more complete snapshot would help. Uncertainty on the absorption mechanism is mentioned in the report itself when commenting on the wide variations in NAD+ observed among the 8 participants:
The current study demonstrates that the apparent oral bioavailability of a 1000 mg dose of NR was highly variable among individuals. While half of the participants showed a significant increase (≥ 100%) in peak blood NR concentration during the pharmacokinetic portion of the study, the remaining subjects showed no or only modest (≤ +50%) changes in blood NR levels. The explanation for this inter-subject variability in post-dose NR levels is not obvious. The instability of NR in blood samples observed here as well as in prior studies [19] could be one contributing factor, although it cannot account for all the variability given the steps we have taken in minimizing instability during handling and processing of blood samples. Another possibility is that, based on its hydrophilicity (XLogP3 = –1.8) [20], NR is expected to exhibit low passive permeability across the human intestinal mucosa. Oral absorption of NR may rely on an active, mediated transport process that varies in active between individuals. It is also possible that NR is degraded to nicotinamide in the gut; nicotinamide is then absorbed and converted to NMN, which can further be converted to NAD+ or dephosphorylated to NR. If true, the degradation of NR to nicotinamide in the gut, which presumably involves purine nucleoside phosphorylase in mammalian and bacterial cells [21] may be a variable step involved in the oral intake of NR. Hence, investigation into the mechanism(s) of NR absorption and metabolism may afford insights into its variable oral bioavailability.
This rat study, btw, suggests their last speculation is closer to the correct one. The significance of this is that if nr is not directly absorbed, then bioavailability cannot be determined by simple bloodstream measurements and AUC calculations on nr alone. I agree that comparing resulting nad+ steady-state measurements following similar nr and nmn dosing regimens may be a more significant metric. I just don't think we have enough comparable data on that yet to choose which is more optimal.
Howard
Posted 30 March 2018 - 06:17 PM
You need to study ling liu’s Dissertation.
I'm guessing you're not referring to the Dr. Ling Liu of Georgia Tech whose dissertations are legend in certain circles like quests for new primes, cryptography, bitcoin mining, dos attacks, and gene decoding. ![]()
I assume you're soliciting my thoughts on this study involving a different L Liu.
It seems to pretty much prove the connection and efficacy of NR supplementation and subsequent NAMpt and NAD production. It employed a genetically modified mouse crossbred to knock out a particular NAMpt producing gene and demonstrated that muscle degradation in those mice attributed to NAMpt deficiency could be alleviated by oral ingestion of NR at a concentration of 12 nm which I think is .012 moles/liter. It's mentioned elsewhere that they believe this achieves approximately a 400 mg/kg daily which I assume is not an unreasonable guesstimate of their ad libitum administration via drinking water... in any event I don't see them drawing any unfounded dosage dependent conclusions other than knockout mice drinking that concentration in all of the water they drink works.
One interesting observation it makes regards bloodstream measurements:
... oral NR dosing increased circulating NAM ~40-fold while NMN remained unchanged and NR was detected only at trace levels in the blood. Thus, the majority of the orally administered NR that reaches the muscle appears to enter in the form of liberated NAM or as NMN
Which seems to reduce the significance of bloodstream NR or NMN levels and reinforces my previous thoughts on that. The mention of NMN clearly adopts the generally accepted NR-NMN conversion cycling which is also illustrated in their graphics. And kind of suggests that a bloodstream summation of NAMpt, NAM, and NMN levels may be more reflective of eventual muscle effects with NAM levels being the most dominating. As the study only tested NR ingestion, it does not shed tremendous light on whether it might be more or less efficient than NMN ingestion. I do note, however, that one NMN study I mentioned earlier does show small but pronounced bloodstream peaking of NMN. Where this NR study found no change.
Howard
Posted 31 March 2018 - 12:16 AM
You need to study ling liu’s Dissertation.
I'm guessing you're not referring to the Dr. Ling Liu of Georgia Tech whose dissertations are legend in certain circles like quests for new primes, cryptography, bitcoin mining, dos attacks, and gene decoding.
I assume you're soliciting my thoughts on this study involving a different L Liu.
No. While he is referring to that Dr. Liu, he's referring to "Liu's dissertation," not that earlier, published paper. I linked it and alluded to it in the opening paragraph of my post, after it had been argued back and forth earlier up in the thread, starting here, but in isolation from the additional studies I brought to bear on the subject. Consistent with the Ratajczak paper and Canto & Auwerx, they find NR to raise tissue NAD+ more than NMN at the same mg dose. The consistent general pattern in all of these papers, along with (secondary) supporting data from other papers I discussed, is why I think, with respect, that digging into the weeds about speculation on the metabolic fate of ingested NR is at this point a bit of an (unintended, of course) red herring.
Posted 31 March 2018 - 12:20 PM
No. While he is referring to that Dr. Liu, he's referring to "Liu's dissertation," not that earlier, published paper. I linked it and alluded to it in the opening paragraph of my post, after it had been argued back and forth earlier up in the thread, starting here, but in isolation from the additional studies I brought to bear on the subject. Consistent with the Ratajczak paper and Canto & Auwerx, they find NR to raise tissue NAD+ more than NMN at the same mg dose. The consistent general pattern in all of these papers, along with (secondary) supporting data from other papers I discussed, is why I think, with respect, that digging into the weeds about speculation on the metabolic fate of ingested NR is at this point a bit of an (unintended, of course) red herring.
What is still interesting I think is whether it would be beneficial to get more or a higher concentration of NR into circulation. At least a higher (peak) concentration I would argue might be achievable with sublingual administration.
Posted 31 March 2018 - 02:54 PM
No. While he is referring to that Dr. Liu, he's referring to "Liu's dissertation," not that earlier, published paper. I linked it and alluded to it in the opening paragraph of my post, after it had been argued back and forth earlier up in the thread, starting here, but in isolation from the additional studies I brought to bear on the subject. Consistent with the Ratajczak paper and Canto & Auwerx, they find NR to raise tissue NAD+ more than NMN at the same mg dose. The consistent general pattern in all of these papers, along with (secondary) supporting data from other papers I discussed, is why I think, with respect, that digging into the weeds about speculation on the metabolic fate of ingested NR is at this point a bit of an (unintended, of course) red herring.
What is still interesting I think is whether it would be beneficial to get more or a higher concentration of NR into circulation. At least a higher (peak) concentration I would argue might be achievable with sublingual administration.
Posted 04 April 2018 - 07:53 PM
I think its worth keeping in mind that putting NR directly into the bloodstream may or may not increase general bioavailability. That may depend on what part of the bloodstream it goes into.
For instance, the study that detected NR peaking in the bloodstream noted that no NR was found in the plasma portion.
It should also be noted that we did try to measure NR in the plasma fraction of a few blood samples obtained from volunteers following ingestion of NR, but failed to detect measurable levels of the riboside. We concluded that NR is concentrated in the cellular fraction of blood.
Since the plasma portion of the bloodstream delivers most of the nutrients, the peaking they measured may only affect the health of the blood cells it occurs in, not NAD levels elsewhere. I would expect that sublingual, trans-dermal, and subcutaneous delivery might put NR into the plasma but I don't think there's any data on whether that might be better than putting metabolites like NAD+ there indirectly following oral NR and NMN ingestion which seems to be readily effective in certain people.
The big question in my mind is why some people measure NAD+ levels over 300% higher than others following oral ingestion of NR. As illustrated in the chart of the 8 participants in this same study:
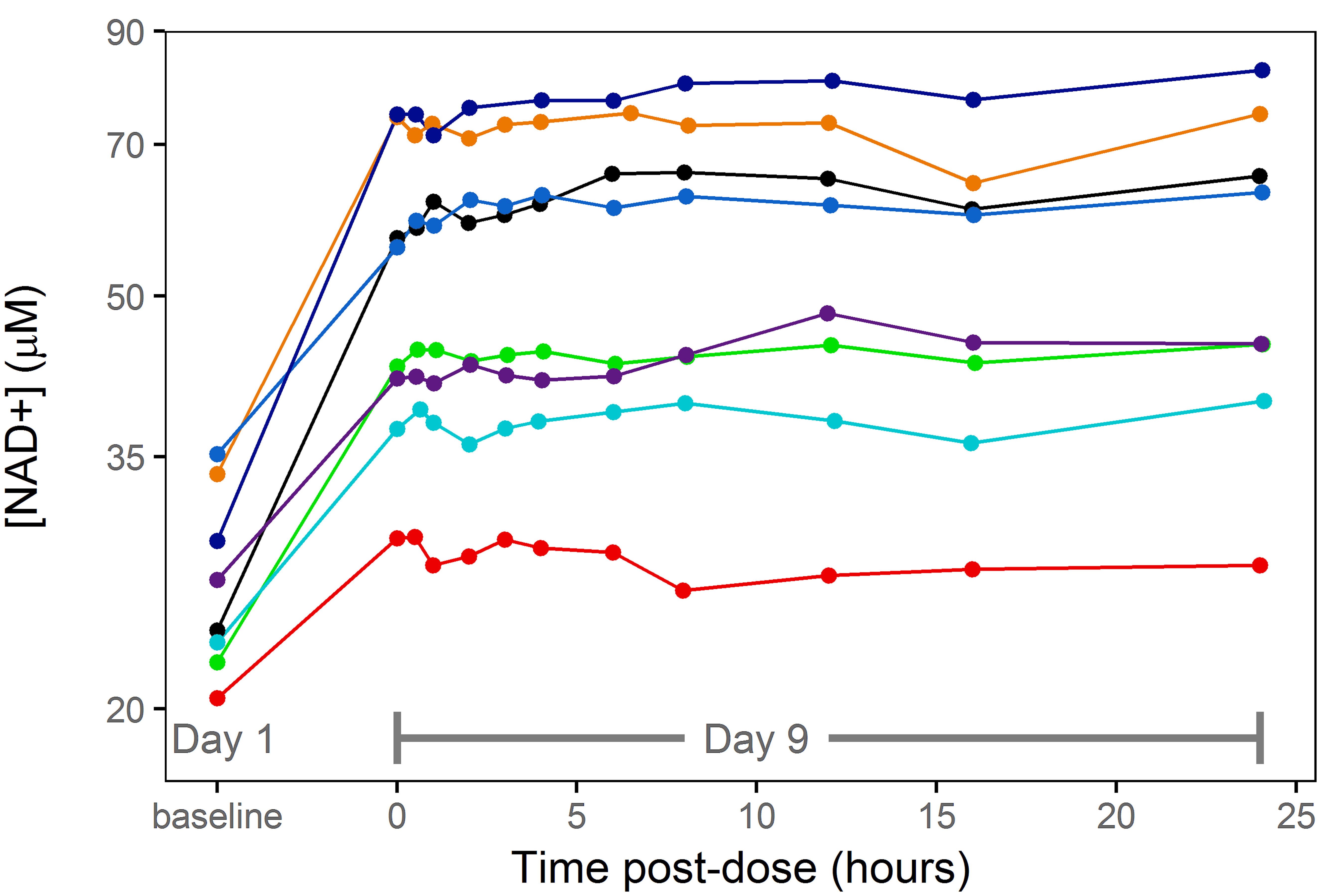
That's a really big spread. Even if you ignore the red one as an outlier, there's still over a 100% variation among those remaining with no apparent clustering but some noticeable pairing (are those couples?). Makes me think there may be very influential environmental impacts on bioavailability... my guess would be diet. More specific possibilities might be exercise patterns, gut flora, gut enzymes, or dietary fiber. Blood glucose levels may also be important. Maybe even particular fad diets. Whatever it is, if we knew the answer we might get the most bang for the buck avoiding the red participant's lifestyle and aiming to emulate habits of the dark blue one on top.
Howard
Edited by hav, 04 April 2018 - 07:55 PM.
Posted 04 April 2018 - 08:15 PM
I think its worth keeping in mind that putting NR directly into the bloodstream may or may not increase general bioavailability. That may depend on what part of the bloodstream it goes into.
For instance, the study that detected NR peaking in the bloodstream noted that no NR was found in the plasma portion.
It should also be noted that we did try to measure NR in the plasma fraction of a few blood samples obtained from volunteers following ingestion of NR, but failed to detect measurable levels of the riboside. We concluded that NR is concentrated in the cellular fraction of blood.
Since the plasma portion of the bloodstream delivers most of the nutrients, the peaking they measured may only affect the health of the blood cells it occurs in, not NAD levels elsewhere. I would expect that sublingual, trans-dermal, and subcutaneous delivery might put NR into the plasma but I don't think there's any data on whether that might be better than putting metabolites like NAD+ there indirectly following oral NR and NMN ingestion which seems to be readily effective in certain people.
The big question in my mind is why some people measure NAD+ levels over 300% higher than others following oral ingestion of NR. As illustrated in the chart of the 8 participants in this same study:
That's a really big spread. Even if you ignore the red one as an outlier, there's still over a 100% variation among those remaining with no apparent clustering but some noticeable pairing (are those couples?). Makes me think there may be very influential environmental impacts on bioavailability... my guess would be diet. More specific possibilities might be exercise patterns, gut flora, gut enzymes, or dietary fiber. Blood glucose levels may also be important. Maybe even particular fad diets. Whatever it is, if we knew the answer we might get the most bang for the buck avoiding the red participant's lifestyle and aiming to emulate habits of the dark blue one on top.
Howard
Posted 04 April 2018 - 09:19 PM
They just didn’t have a sensitive method to measure NR. Ling Liu’s Dissertation dectectes NR at baseline that is much higher than baseline NMN. But the portion of NR that gets into blood stream intact is still small. So they need to do another study to check on sublingual and other delivery methods. Getting more NR into other organs other than liver will probably provide more benefits for these organ’s than just recycled NAM. So I expect NR will be more effective when better delivery methods are available.
Just looked at her Chemistry Department dissertation and it's not totally clear what portion of the blood she tested. "Whole blood" is mentioned once but there is no mention anywhere of centrifuging it to separate the cells from the plasma. The problem generally cited isn't so much the sensitivity of the test but that NR in drawn blood degrades so quickly that even if it is there, it might be gone by the time its done centrifuging to separate out the plasma. There is mention of immediately flash-freezing the blood to avoid this degradation but the plasma cannot be separated in that state.
Howard
Posted 04 April 2018 - 10:02 PM
They just didn’t have a sensitive method to measure NR. Ling Liu’s Dissertation dectectes NR at baseline that is much higher than baseline NMN. But the portion of NR that gets into blood stream intact is still small. So they need to do another study to check on sublingual and other delivery methods. Getting more NR into other organs other than liver will probably provide more benefits for these organ’s than just recycled NAM. So I expect NR will be more effective when better delivery methods are available.
Just looked at her Chemistry Department dissertation and it's not totally clear what portion of the blood she tested. "Whole blood" is mentioned once but there is no mention anywhere of centrifuging it to separate the cells from the plasma. The problem generally cited isn't so much the sensitivity of the test but that NR in drawn blood degrades so quickly that even if it is there, it might be gone by the time its done centrifuging to separate out the plasma. There is mention of immediately flash-freezing the blood to avoid this degradation but the plasma cannot be separated in that state.
Howard
Posted 04 April 2018 - 10:05 PM
I also agree. The current state of science doesn’t tell the full story of NMN either.
Posted 04 April 2018 - 10:32 PM
Agreed on both counts. Good point Howard.
Edited by TMNMK, 04 April 2018 - 10:33 PM.
Posted 04 April 2018 - 10:32 PM
Science & Health →
Supplements →
NAD+ →
NR and NMN optimum doseStarted by MikeDC , 11 Nov 2020 |
|

|
||
Science & Health →
Supplements →
NAD+ →
NMN didn’t raise neonatal mouse brain NAD+ when injected intraperitoneallyStarted by MikeDC , 23 Apr 2020 |
|

|
||
Round Table Discussion →
Business →
Retailer/Product Discussion →
Nr and NMNStarted by Grim Reaper , 29 Aug 2014 |
|

|
0 members, 2 guests, 0 anonymous users