Stack Submitter
Stack Details
- Submitted: Aug 22 2017 09:42 PM
- Date Updated: Sep 04 2018 06:08 PM
- Views: 21523
Michael's "Tiered" Supplement
Description
Moved to action by the slow trickle of people occasionally asking for an update to my 2006, 2009, and 2012 supplement regimens, and the stimulus of the contest, this is my current supplement regimen.
On supplement use in general, I would still recommend my 2004 CR Society Conference lecture, which has held up pretty well. Notable changes in the science: I said then that there was "No confirmed evidence for life-extending effects of any drug or supplement in normal, healthy mammals," whereas we now have extremely convincing evidence for rapamycin, and pretty promising results for acarbose as well — albeit in males only.(1,2) On the other hand, a lot of the things that had seemed promising back then (lipoic acid, metformin, resveratrol(3-5a)) have subsequently proved illusory. The general finding of supplements failing to extend LS in well-done animal studies and protect against chronic disease in clinical trials has continued, as has the finding of unexpected side-effects of megadose supplementation.
I still find it useful to conceptualize supplements in three tiers, in decreasing levels of priority and increasing levels of uncertainty and risk: Tier 1: Correct Deficiencies (by which I mean real, actual deficiencies, per the National Academy of Medicine's DRIs); Tier II, Disease Risk Reduction (I might today divide this into Tier IIa: risk reduction for diseases for which one is at specific risk, and IIb: disease risk reduction for things at which one is at average or lower-than-average risk: the former is more biologically plausible and has a better track record in epidemiology and clinical trials); and Tier III, Life-Extension Supplements. The record on Tier IIb is pretty poor, and the record on Tier III is really awful: I mentioned lipoic acid, metformin, and resveratrol(3-5a) above: the 2004 Tier III page also lists pyridoxamine — another flunk, even on its narrow indication for inhibiting AGE-related pathology and metabolism,(14,15) let alone life extension.
The most important thing you can do as regards supplementation is to actually use nutrition software such as CRON-O-Meter to get a handle on your actual dietary intake of essential nutrients before deciding what to supplement, tho' this is less of an issue to the extent that your diet is (a) genuinely poor (& thus more likely to actually need 'everything' and not be overdosing on eg Mn, Cu, etc) and (b) you're not on CR (and thus have a lot of 'slop factor' and don't have the specific nutritional risks of CR folk). (Yes, ironically, health-conscious people actually have more need for caution in supplementation, because they often wind up on somewhat restrictive 'health food' regimens that limit the diversity of their nutrient sources, and because it's common for people eating quite well to get too much of some nutrients from diet alone, and then add supplements on top of that. Studies show, perversely, that the people who need vitamin supplements the most use fortified cereals the least -- and the converse). A 2-week representative COM crunch of my diet is appended; see also this detailed post on my quotidian diet).
Do also make use of the relatively few reliable functional diagnostics for nutrient deficiency, such as serum 25(OH)D3 for vitamin D (target range should be 30-40 ng/mL — vide infra), homocysteine and MMA for vitamin B12, ferritin (and, if your levels are low, in combination with Total Iron Binding Capacity; Unsaturated Iron Binding Capacity; and Transferrin/Transferrin Saturation).
Veg(etari)ans should also see my post on nutritional supplementation for vegetarians for issues of specific concern to them, not all of which are obvious from a COM readout.
By now, everyone should be thoroughly disabused of the "it can't hurt, and it might help" heuristic of supplementation: we've seen time and time again that supplementing more than a few mutliples of the RDA for essential nutrients causes real or likely harm, from high-dose selenium raising the risk of diabetes (and possibly some cancers), to the possible increases in lung cancer mortality amongst smokers supplementing with beta-carotene (when the trial was based on epidemiology associating high dietary beta-carotene with reduced risk of lung cancer amongst smokers), to increased mortality in mice administered a human-equivalent full dose of Life Extension Mix®,(41) and other cases discussed in my 2004 presentation — as well as concerns that are not yet confirmed but that merit caution, such as the potential cancer-promoting effect of folic acid and the hypothetical cancer promoting effect of benfotiamine and other high-dose or high-bioavailability forms of thiamine.
This is put very well in Oakman's "pothole theory" of supplementation:
If you don't have a 'hole' in your metabolism, meaning a diminished ability to produce something due to age or malfunction, or lacking it altogether, supplementation isn't unlikely to help. Plus, you only need enough to fill the 'hole,' not more (i.e., a "bump" is as bad as a "hole").
On this point, let me emphasize the logical corollary which I've spelled out repeatedly but that people keep missing: unless your diet is composed entirely of fries, Coke, and fast-food burgers with the lettuce, ketchup, and tomato thrown out, no one should be taking a full daily dose of any commercial multivitamin. You are absolutely guaranteed to get too much of many nutrients, and to create or exacerbate imbalances in others.
This, then, is a regimen for a very specific individual: a very healthy, young(ish) lacto-ovo vegetarian CR practitioner with an excellent diet (which I've analyzed extensively, to understand its weaknesses and "excessive" strengths -- see a representative week's average appended to this post). As the links above indicate, a person must customize hir regimen based on hir own diet, and also age, specific risk factors, existing diseases, etc.
So: the regimen (notes on WHY I take various things at the end, when it isn't obvious from the link or other grounds):
UPON WAKING (5 AM or before), w/coffee:
1/2 tsp (1.8 g) CreaPure Creatine monohydrate (do not buy commodity creatine! See below).
314 mg Strontium (citrate)
5:50 AM, with green tea
500 mg AjiPure L-Lysine
1 Prostaphil defined pollen extract
6:30 AM, breakfast:
{I would be taking Provinols,if I could find them ... see below}
500 mg AjiPure L-Lysine
1 g Beta-alanine
420 mg Phosphatidylcholine
250 µg Methylcobalamin
25 mg pyridoxine
75 µg Iodine (1/3 of 225 µg tablet)
250 mg nicotinamide riboside (NR) (skip on Fridays)
While scrubbing teeth: 1 drop per eye N-acetyl-L-carnosine eyedrops
10:30 AM, with coffee:
1500 mg glucosamine sulfate
11:10 AM, with green tea:
Brain nutrient (rotating one of: 800 mg piracetam ( why?) (once/wk), pyroglutamate (500 mg, thrice/wk), and extra creatine (on resistance training days)
11:50 AM, with green tea:
500 mg AjiPure L-Lysine
12:30 PM, lunch:
500 mg AjiPure L-Lysine
1 g Beta-alanine
420 mg Phosphatidylcholine
1000 mg AjiPure Taurine
30 mg CoQ10
15 mg Menatetrenone
125 mg NR (skip on Fridays)
1 mg Lithium (orotate -- do see note below!)
4:30, with green tea:
1 Prostaphil
5:10, with decaf coffee:
500 mg TryptoPure tryptophan
5:50, with green tea:
500 mg AjiPure L-Lysine
6:30, dinner:
500 mg AjiPure L-Lysine
1 g Beta-alanine
500 IU (average) vitamin D3 (as 1 x 1000 IU softgel, 3 d/wk in summer and 4 d/wk in winter)
750 mg taurine
22 mg zinc (picolinate)
1 Rite Aid B-Complex With B12
420 mg Phosphatidylcholine
10 pm, bed
(Rarely) 750 mcg melatonin (jet lag)
Further on Rationales
Strontium: I have low BMD typical of natural- and CR-induced low BMI; this is a fracture risk factor, tho' not as much as would be routinely assumed and even diagnosed, because of my overall risk profile: see the new FRAX fracture risk assessment tool developed by the WHO. See also this post on how CR appears to protect bone against age-related decline in bone quality/microarchitecture, for which the available human evidence is now in support, or at least to which it offers no contradiction.(35) Strontium is one of the best-documented supplements on the planet, having been shown in multiple clinical trials to actively increase bone formation, raise or maintain BMD, and reduce fracture risk (in post- or peripausal women, NB, whose bone loss is for very different reasons and is associated with decay of bone architecture).
Creatine, beta-alanine, taurine, zinc: I'm lacto-ovo vegetarian for my quotidian diet, and am therefore somewhat low on these, and Vegetarian Booster has been discontinued. See again my post on supplementation for veg(etari)ans. However, I don't take ALCAR: like free choline, can be metabolized into TMAO by gut bacteria,(36,49) going thru' γ-butyrobetaine in the process;(47,48) something about this process appears to promote atherogenesis even in persons with low LDL and other CVD risk factors ((36,47,48) and other references; see also further discussion under phosphatidylcholine, below). Additionally, altho' ALCAR led to transcriptional changes similar to CR when administered to young mice, it also lowered levels of SIRT3,(40) whereas CR elevates it in flies, mice, nonhuman primates (in the questionable WUSTL study),(42) and (questionably) in humans on intermittent fasting,(42) and is likely important to the benefits of CR (and of NR, if they translate to humans at all — see below).
Creatine: As noted, I'm vegetarian, and our intakes and serum levels are lower than omnivores' (from these three sources, it appears that typical omnivorous dietary intake is 1-2 g/d, and some of that will be unabsorbable due to cooking, unlike high-quality supplemental creatine), and trials seem to show that vegetarians' muscles and (on some tasks) brains work better when given a low-dose supplement(18).
If you use creatine, insist on a supplement made using CreaPure (a branded raw material manufactured by AlzChem AG (formerly Degussa AG Trostberg; formerly SKW) but used in several different retail brands). Around the turn of the century, Dr. N..... at A0R had raised concerns about contaminants in other creatine manufactrers, but I didn't look into it at the time as A0R wasn't marketing it and I wasn't taking it. Several years ago, however, I bought some creatine from a company that I generally consider to be reputable and from whom I often buy commodity-item supplements, and was disturbed by its very bitter and (surprisingly) soapy taste. I called the company, who dug back thru' their QC procedures and retained sample, and insisted that it was fine.
Unconvinced, I started digging around, and found that there are indeed reasons for caution, as outlined in these two very good articles on creatine by Will Brink: "What's in your Creatine?" and "What's Really in Your Supplements? - An Update on Creatine"; see also Alzchem's CreaPure promotional materials, and (39). I proceeded to order some CreaPure-sourced creatine and was surprised that, for the very first time with any creatine supplement, the stuff had absolutely no bitter taste to it: the suspicious supplement had been the first one I'd ever used with the weird a soapy taste, but every creatine I'd previously used had a mild bitterness to it, which I'd thus assumed to be intrinsic to creatine itself, whereas it now seems it is rather the taste of some impurity.
There is no direct evidence that dicyandiamide or dihydrotriazine is harmful — but why anyone (let alone a life extensionist!) would knowingly put high (relative to likely dietary intakes) levels of organoleptically-detectable impurities of unknown toxicity into hir body to save a few dollars is beyond me.
Also, do read this sensible safety caution about the long-term effects of creatine supplement use (skip down to"Risks/side-effects of creatine use"), much of which applies to many other supplements.
Beta-alanine: I was previously taking carnosine, which is extremely low in vegetarian diet, and studies show that vegetarians have lower levels of carnosine in thier muscles than omnivores.(44,45) However, I've now substituted beta-alanine, which does a better job of elevating tissue carnosine levels (and increases muscle power per se in the surprisingly large number of controlled trials that have been done on the stuff; although this wasn't my main reason for taking it, my anecdotal experience is happily consistent with the trials). I take it with meals to maximize tissue uptake and retention.(46) Be careful to ramp your dose up slowly. Bottle directions often suggest 1.5 or 2 g, 4 x daily, but that's the final, ramped-up dose used in the trials; however, if you start out at that dose, you're likely to suffer maddening paraesthesia (pins and needles), as explained here. Instead, start at 500 mg 4 x daily, and work your way up as needed or desired. I take a lower dose than he dose used in most trials as an ergogenic aid out of caution about what's causing the paresthesia.
Prostaphil defined pollen extract: I have an idiopathic urinary urgency; definitely not BPH or bacterial prostatitis, conceivably related to alpha-adrenergic function. This is subjectively very helpful.
Iodine: Getting reliable information on iodine intake is very difficult. As a vegetarian, my intake is probably low, and I do consume a significant amount of cruciferous veggies, which inhibit iodine uptake by the thyroid. I'd strongly caution against using "sea vegetables" as a source, because iodine levels in same can be EXTREMELY high: in particular, kombu kelp can savage your thyroid gland. Moreover, unfortunately most iodine supplements are kelp-derived and high-dose -- and occasionally unreliable or contaminated with arsenic. The NOW supplement I link above serves my purposes well.
Menatetrenone: As noted, I have low BMD typical of natural- and CR-induced low BMI; Menatetrenone (menaquinone-4 MK-4 – a form of vitamin K2, but different from the cheaper menaquinone-7) has been shown to reduce the risk of fractures in a variety of settings (mostly postmenopausal osteoporosis) and seems promising for CR-related low bone mass, as menatetrenone primarily appears to reduce risk by preserving bone quality rather than quantity -- a more likely viable strategy for a person whose actual mass of bone is constrained by low energy intake. There are some trials showing favorable effects of menaquinone-7,(eg. (54,55) but none have actually shown it to reduce fracture risk (unless you count vertebral deformities).
AgiPure lysine: This has been found to be surprisingly effective in reducing AGE and AGE-induced complications of diabetes, especially in the kidneys but also apparently in the heart (6-8). (13) was negative, but the measurement of AGE was in skin, which not be reached by a significant concentration of these nutrients (vs the heart and kidneys, thru' which they would of course travel in the blood when they're taken on an empty stomach), and their conclusion was (reasonably) that "treatment may need to continue for more than 1 year before clinical status improves." AgiPure sourcing: After first my creatine experience (above), I subsequently had a quite similar experience with Ajinomoto's AjiPure Glycine, which I was taking at the time: the taste of their product is sweeter and 'cleaner' than any other brand of glycineI've used. Because I'm now consuming 3 g of lysine a day, and with the knowledge of the impurities underlying the bitter taste in commodity creatine, and in recollection of the tryptophan-related outbreak of eosinophilia-myalgia syndrome (EMS) in 1989, I switched from commodity lysine to Ajinomoto's AjiPure L-Lysine (and similarly AjiPure Taurine).
Provinols: the only authentic red wine concentrate, which I would take if I could find if I could find the darned stuff. Unlike the shaky-to-begin-with-and-now-disproven resveratrol hype, there is a quite solid body of epidemiological evidence of an association between a couple of glasses of wine a day and lower risk of a range of adverse outcomes, including total mortality and dementia. The epidemiology clearly indicates a U-shaped dose-response curve for alcohol consumption and heart disease, with the best outcomes associated with 1-3 drinks/d, and this extends to total mortality in meta-analysis(19); but when broken down into type of alcohol consumed, only wine lowers total mortality and dementia: beer or spirits lower CVD mortality, with no effect on total. (No, despite the use of these findings as a justification for resveratrol supplements, there is no epidemiological evidence favoring red over white). The benefits for total mortality reach a nadir at < 1 5 oz glass of wine per day.

Figure 1. Relative risk of total mortality (95% confidence interval) and total alcohol intake extracted from 56 curves using fixed- and random-effects models. From (19).
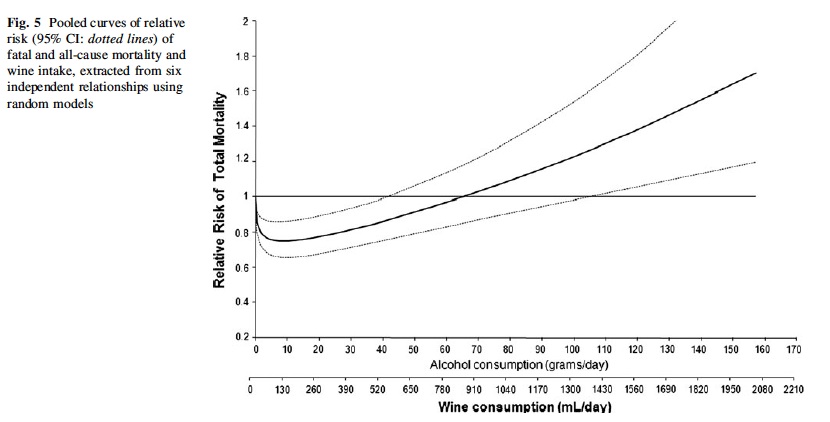
Wine consumption vs. total mortality. From (38).
However, my working hypothesis is that the climbing risk is due to the toxicity of alcohol per se, and that additional benefits might be available from higher intake of the component(s) of wine responsible for these benefits, without the extra Calories and toxicity of drinking the stuff. However, we don't know which component(s) of wine exert these effects, so we should aim for a supplement that is a direct concentrate of the same spectrum of bioactives in actual, fermented wine. Provinols is the only supplement Ii've found that fits the bill: every other "red wine extract" I've found turns out to be, upon further investigation, grape seed and/or skin extract, with or without added resveratrol. The mix of phenolics in grape seed and/or skin is actually quite different from that in wine, due to complexation and biotransformation that the grapes undergo during fermentation. Seppic in France has done a great deal of work in characterizing these, and still the surface is only barely scratched and we don't know what might do what.
Therefore, I went looking for a genuine concentrate of actual red wine that did not rely on high temperature or extraneous chemicals which might also alter the original mix, and which did not come from China or another country with high levels of industrial contaminants or shady business practices. I first hit on Provinols, which is a pioneering product in this field, but unfortunately it is damned near impossible to get in the Americas, except in low doses and mixed in with other junk. (Europeans and Turks may be able to get it, however). I was at one time convinced of the authenticity of a product called Wine Rx, but they subsequently failed to document their claims on composition, and moreover, it seems to go vinegary and weird in well less than a year -- not surprising perhaps, granted that it was only a 50% extract. So, I await glumly for the Real Deal.
Phosphatidylcholine: Replaces citicoline and free choline supplements, which may promote atherosclerosis (see also here). See also here on free vs. phosphatidylcholine supplementation and supplemental phosphatidylcholine contamination. In addition to studies covered in those links, there are the results of a recent short-term human trial:
healthy vegans/vegetarians (n=8) and omnivores (n=10) with no preceding (1-month) history of antibiotics or probiotics ... (46±5 years of age, 40% male, nonsmokers without hypertension, diabetes mellitus, or cardiovascular disease) were given oral choline supplementation (choline bitartrate 500 mg twice daily, ≈450 mg total choline/day) for 2 months ... Both vegan/vegetarian and omnivore alike showed significant >10-fold increases in plasma TMAO levels at both 1- and 2-month periods (P<0.01 each; Figure, A), with corresponding enhanced platelet aggregation responses to submaximal adenosine diphosphate (5µM) after choline supplementation (Figure, A). Moreover, a striking dose-dependent association was observed between plasma TMAO levels and platelet function

There's clearly a significant amount of variation in the effect, including the differential effects in veg(etari)ans vs. vegans seen above and in several of this group's previous studies; it's clear that gut bacteria play a central role (10-12). An attempt to fix this with probiotic supplementation failed: L. rhamnosus actually elevated TMAO production in mice.(12)
I'm aware that this is contentious. To briefly debunk an argument advanced by the Weston A. Price Foundation and Chris Kesser: the fact that fish is high in TMAO and yet its consumption is linked to lower risk of cardiovascular events is irrelevant: (a) TMAO itself may be only a marker of some process involving the metabolism of methylamines by gut bacteria and/or the liver by FMO3 (including but not limited to the resulting lowering of choline availability due to its bacterial consumption (10a)), in which case preformed dietary TMAO may be irrelevant; and (b) it's possible that the benefits of fish come are net effects, with (eg.) the taurine, omega-3 fatty acids, and displacement of red meat from the diet being all positive, and the TMAO content negative, with the positive outweighing the negative. (Citicoline(50) and carnitine(36,47-50) also generate TMAO, NB, and alpha-GPC very likely also does).
Choline is, in any case, an essential nutrient, so you have to get it: even if you're skeptical of the causal relationship, it merits erring on the side of caution by avoiding free choline salts in favor of PC from a reputable, high-turnover supplier. Note that phosphatidylcholine is only 13% free choline by weight, so eg 420mg of phosphatidylcholine is only ~55 mg free choline (thanks Sillewater!). Note also that the USDA choline database only includes 630 foods, so one's real intake is certainly higher than what nutrition software indicates — but don't let this make you overconfident of adequacy. Elevated serum creatine phosphokinase (CPK), aspartate aminotransferase (AST), alanine aminotransferase (ALT), or lactate dehydrogenase (LD) may in some cases indicate choline deficiency, tho' (a) they can be elevated for unrelated reasons, and (b) I'm not clear on how severe one's deficiency has to be before noticeable elevations will occur.
Methylcobalamin and B6: I had previously taken only a very low dose of B12 (15 µg (1/6 of a 100 µg vitamin B12 tablet)) and no B6, but found that my homocysteine was rising — first slowly, and then rather suddenly. I suspect a lot of this is having taken up coffee consumption, which does raise homocysteine (and I am pretty sure that my series of high tests was the result of having consumed (black, unsweetened) coffee before going in for my blood draw), but may also relate to changes in demand for transsulfuration under CR (see below under taurine). After trying a few other things, including extra low-dose B vitamins as Rite Aid B-Complex With B12 (below), I finally added these, and my homocysteine is back down to normal. It must be said that the evidence for homocysteine really being causal in age-related disease — and, in particular, the track record of dietary supplements to lower it being effective prevention against such — is weak at best; however, I'm not willing to take the risk.
Nicotinamide riboside: Yes, I admit it
The first and biggest problem looming over nearly all the NR research is that it was done in C57BL/6J mice, who carry a characteristic mutation in the NNT gene, which makes the translatability of any study based on NAD+ repletion questionable. The NNT mutation leads to inadequate reduction of NADP+ in their mitochondria, resulting in elevated mitochondrial oxidative stress and less efficient ATP production. One possibility is that megadose NR partially offsets this defect by augmenting the cellular level of NAD+, facilitating a more normal level of NADP+ reduction to NADPH. By contrast, in an animal with an intact NNT gene (such as a rat (as in this study showing NR reduced exercise performance by 35%), or the C57BL/6JRcc mice used in this study, or the vast majority of humans) — in such an organism, increasing the level of NAD+ via megadose NR might instead disrupt optimal NADP:NADPH redox coupling, leading to functional impairments. (See my extensive discussion of the NNT mutation and nicotinamide riboside/NMN research).
Above and beyond this, the NR lifespan study (16a) has additional problems. Mice administered NR at 400 mg/kg commencing at 24 months of age (relatively late in life) enjoyed "slightly increased [median] lifespan (chow diet, mean 829 ± 12.0; NR, mean 868 ± 12.4 days, p = 0.034) (Fig. 6G)" — anincrease in overall median lifespan from birth of 4.7%. The authors don't report maximum (tenth-decile) survivorship, an increase in which relative to normal, healthy controls is the sine qua non of an anti-aging intervention, but looking at the survival curves, the very last control animal died at age ≈960 days (700 days (see legend to Figure 6) + an eyeballed 260 d from the graph)), and the last treated animal died at age ≈1010 days — a similar increase of 5.2%, albeit a much dodgier figure. But as I've pointed out many times before, a normal, healthy, well-husbanded, non-genetically-messed-up mouse will on av'g live ~900 days , and 1100 days at maximum (tenth-decile survivorship). But in report after report of 'life extension' in mice — including this one — not one of the animals lived even this long, let alone enjoying a true extension of healthy life.
Now, I don't know exactly what went wrong in this study: it could just be the result of not having enough mice in the study (n = 30 per treated group; you really want n=50), or diabetic obesity from overfeeding (animals were given literal ad libitum access to diet and water, whereas well-done lifespan studies restrict the animals 10-15% to avoid obesity) or malnourishment, or failing to keep a good lid on pathogens ... something went a bit off in this experiment, resulting in modestly short-lived controls, and more or less normal treated animals. This is also clear just from looking at the shape of the survival curve itself, which is clearly not rectangular: from ≈850 days onward, both groups were clearly suffering abnormal early attrition:

So this doesn't actually show an increase in LS, but rather a partial normalization of LS in a slightly short-lived colony: they limped along better for their abnormally short lives.
Additionally, it was done in C57BL/6J mice, who carry the NNT mutation, as discussed above.
The Imai "aging" study (16) is also questionable, both because they also used C57BL/6J mice, and because the mice were not allowed to live long enough to get particularly old: they initiated treatment at age 5 mo, which is like a human in hir mid-20s, and extended to 17 mo, which is maybe 50 human years old. It'd've been more convincing and translatable if they had started in midlife and extended it to 24 mo or beyond.
There is also some reason to be concerned that megadosing any NAD precursor such as nicotinamide riboside might fuel the progression of some cancers.
There is also the concern that megadosing NAD precursors (nicotinic acid <NR< nicotinamide (26)) results in the generation of N-methylnicotinamide (NMNT or MeNAM), which may have deleterious effects on metabolism and neurodegeneration, including diabetes,(27-27g) obesity,(27,28) Parkinson's disease,(29,30) and coronary artery disease.(31) The strongest case is the finding in clinical trials that nicotinic acid modestly increases the risk of diabetes in clinical trials;(27g) if NMNT is the culprit, you would expect NR to be more risky for this than nicotinic acid, since it raises NMNT more.(26)
("But wait!" you say. "NR has been shown in several studies to prevent or partly reverse diabetes!" Yes, but those studies used C57BL/6J mice with the NNT mutation, where you'd expect that NAD precursors would improve the impaired glucose tolerance caused by the mutation by eg. reducing oxidative stress in the beta-cells and increasing metabolism. Human clinical trial results are a much more inherently powerful source of data for humans, an must not be ignored).
And, in general, our understanding of NR and NAD metabolism is a lot cruder than people on this Forum seem to believe: see the very useful review by Chini et al.(34)
It's also worth remembering that plain-jane nicotinamide has been reported to have many of the same effects reported breathlessly for NR, such as against animal models of diabetic obesity, stroke, and Alzheimer's.
I chose a dose that based on Trammel & Brenner(26) seems to raise PBMC NAD+ substantially, without the huge rise in MeNAM seen at 1000 mg. I skip NR on Fridays in order to give my system at least some space to clear out MeNAM; plus anecdotally, my sleep seems to go haywire if I don't.
Glucosamine sulfate: No, I don't have any kind of arthritis or other joint problems. Glucosamine appears to slightly extend the lifespan of middle-aged mice,((49), although they only report tje survival curve and statistical significance of the differences in mean (?) and maximum lifespan in the mice, without giving the mean and maximum lifespans of the various groups quantitatively — and the survival curve suggests a lot of early mortality): (51)

Additionally,
Current use of glucosamine was associated with a significant decreased risk of death from cancer (HR 0.87 95% CI 0.76-0.98) and with a large risk reduction for death from respiratory diseases (HR 0.59 95% CI 0.41-0.83) (Pocobelli et al., 2010; Bell et al., 2012). Glucosamine supplementation [was associated with a] decrease risk of lung cancer in humans (Brasky et al., 2011). A meta-analysis has shown that glucosamine has lowest risk of adverse effects compared with other treatments (Diarecin and NSAIDs) (Kongtharvonskul et al., 2015). The oral supplementation of glucosamine can potentially improve cutaneous aging in human and reduce the appearance of visible wrinkles and fine lines of the skin (Murad & Tabibian, 2001).(52)
Most of these effects, including that on colorectal cancer, were seen in the VITAL study in Washinton state; the association with reduced colon cancer risk was seen independently in the Nurses' Health Study and Health Professionals Follow-up Study.(53) I recommend glucosamine sulfate 2KCl, not the cheaper glucosamine hydrochloride.
However, prompted by Florin, I have just (2018-07-27) noted two studies (60,61) finding that glucosamine supplementation raises intraocular pressure (IOP), the main driver of glaucoma. (60), which is more robust in design, only finds a rise because of a mixture of a lower baseline (reversion to the mean?) and some post hoc fiddling, and "Although mean rise of IOP was statistically significant in the glucosamine group, more than 2 mm Hg rise in IOP was also more in the treatment group (34% of those receiving treatment vs 12.5% of patients on placebo)." And it was done in Iran.
However, even a suggestion of a risk may not be worth it to some people, especially if their inflammation is already low or they have reason to think they're at risk of glaucoma.
Pyroglutamic acid: See here on piracetam (once/wk and this on pyroglutamate. VRP, my previous source, discontinued pyroglutamic acid. I'm very annoyed: this is the SECOND time they've disc. something I use for which they're the only trustworthy source I know, and w/o notice ... I have yet to find any other source of encapsulated, pure pyroglutamic acid. (S*urce N@turals sucks (a couple of flunked consumerlabs.com tests, totally inappropriate tableting of R-LA, other bad behavior), and I don't want arginine pyroglutamate). I'm currently left buying in bulk and encapsulating it myself. If anyone knows of a reliable source for this supplement, please PM me.
CoQ10: The evidence on what CR does to CoQ levels in rodents is mixed and hard to interpret, but it's reasonable to think that a CR person's levels might be lower, due to natural downregulation of HmGCoA reductase (the enzyme opposed by statins: statin users have low CoQ, as the products of this enzyme are used to synthesize both cholesterol and CoQ). Whether elevating my serum levels with a pill do me any good is a good question, as is whether any decrease in CoQ might be part of the mechanism of CR ...
I take it as ubiquinol. There's some somewhat deceptive reporting on marketed ubiquinol, but I take it in this form rather than regular (oxidized/ubiquinone) CoQ10 on a somewhat superstitious better-safe-than-sorry basis.
Lithium (aspartate or orotate): I just do my best to spread the contents of a 5 mg cap evenly over 5 days. No, this is not the pharmacological dose shown to be neuroprotective in rodents subjected to horrible pharmacological or genetic assault, nor in human disease victims, neither of which are reasonable justification for use (let alone for dosages) in normal, healthy humans. See instead (24), which presents animal studies and a surprisingly large am't of (unfortunately, but of necessity, 'ecological' rather than truly prospective) epidemiology suggesting that Li is an essential nutrient, with an 'RDA' of ≈1 mg, whose presence in the water is linked to having a much happier (less violent, criminal, suicidal, and generally "crazy") population; see also (25) in Japan. More recently, this same Japanese study seems to have documented a non-sneezable increase in life expectancy in the higher-Li-water communities.(32) The source I used to use (guess who
TryptoPure Tryptophan: Originally and primarily for sleep, as a precursor of serotonin and thence melatonin though the evidence on this is actually kind of weak (and that turkey thing is a myth). It's also an NAD precursor. Of interest:
A large number of reviews attribute a marginal role to the de novo NAD+ synthesis pathway. However, a solid support for this claim is lacking. One of the studies frequently cited to sustain this point of view reports that tryptophan alone is not sufficient to maintain the physiological NAD+ concentration of the cell (Nikiforov et al, 2011). However, this conclusion was exclusively based on the observation that supplementation with tryptophan is not sufficient to protect cells from the death induced by NAMPRT inhibitor FK866, and no NAD+ quantification was performed in this study. In addition, some studies show that, at least in the liver, tryptophan constitutes the preferable substrate for NAD+ production. Rat primary hepatocytes, treated with NA, NAM, or tryptophan, were reported to use exclusively tryptophan for their NAD+ biosynthesis, even though they were still able to take up NA and NAM from the culture medium (Bender & Olufunwa, 1988). Administration of tryptophan, NA, or NAM to rats showed that tryptophan resulted in the highest hepatic NAD+ concentrations (Bender et al, 1982). Moreover, it has been shown that in rat liver, NA and NAM have a very limited capacity for NAD+ production, probably due to the saturation of the involved phosphoribosyltransferases, whereas no such limitations were detected for the NAD+ synthesis from tryptophan (Williams et al, 1950; Bender et al, 1982; McCreanor & Bender, 1986).(59)
Zinc (picolinate): my regular diet includes what should be quite adequate zinc, but my dietary copper intake is so high I get copper-induced secondary zinc deficiency if I don't supplement.This was mildly symptomatic for much of the year for several years (Beau's lines (more usually associated with iron deficiency), cracking fingertip skin, inability to taste zinc sulphate heptahydrate solution) when I don't, despite a fairly high dietary Zn, presumably due to high dietary copper), and even the 7 mg/d in the old A0R Vegetarian Booster wan't quite enough to keep it at bay. Of course, most omnivores have if anything the reverse problem.
Vitamin D3:
This is not only one of the most recent, but the methodologically strongest meta-analysis of the relationship between serum 25(OH)D3 levels and total mortality, giving strong evidence that the optimal level for 25(OH)D is ≈75-100 nmol/L [30-40 ng/mL]:
Quote
Vitamin D and mortality: Individual participant data meta-analysis of standardized 25-hydroxyvitamin D in 26916 individuals from a European consortium
Vitamin D deficiency may be a risk factor for mortality but previous meta-analyses lacked standardization of laboratory methods for 25-hydroxyvitamin D (25[OH]D) concentrations and used aggregate data instead of individual participant data (IPD). We therefore performed an IPD meta-analysis on the association between standardized serum 25(OH)D and mortality.
Methods
In a European consortium of eight prospective studies, including seven general population cohorts, we used the Vitamin D Standardization Program (VDSP) protocols to standardize 25(OH)D data. ...
Findings
We analysed 26916 study participants ... with a median 25(OH)D concentration of 53.8 nmol/L [21.55 ng/mL]. During a median follow-up time of 10.5 years, 6802 persons died. Compared to participants with 25(OH)D concentrations of 75 to 99.99 nmol/L [30-40 ng/mL], the adjusted hazard ratios (with 95% confidence interval) for mortality in the 25(OH)D groups with 40 to 49.99, 30 to 39.99, and <30 nmol/L were 1.15 (1.00–1.29), 1.33 (1.16–1.51), and 1.67 (1.44–1.89), respectively. We observed similar results for cardiovascular mortality, but there was no significant linear association between 25(OH)D and cancer mortality. There was also no significantly increased mortality risk at high 25(OH)D levels up to 125 nmol/L.
PMID 28207791
Note that this addresses several complaints (reasonable and not) of megadose D advocates such as William B. Grant and Cedric Garland, including the use of unrepresentative high-risk and/or institutionalized populations in China and elsewhere, the lack of standardization of vitamin D levels, and underpowering. Note, additionally, that this is an individual patient-level data meta-analysis, which is a much stronger design than the more common (and much easier) straight-up mushing together of "high" vs. "low" quantiles from each study, irrespective of the absolute values represented in those quantiles.
We also have the recent null results of a randomized, placebo-controlled clinical trial of vitamin D supplementation against CVD:
Effect of Monthly High-Dose Vitamin D Supplementation on Cardiovascular Disease in the Vitamin D Assessment Study : A Randomized Clinical Trial.
Scragg R1, Stewart AW1, Waayer D1, Lawes CM1, Toop L2, Sluyter J1, Murphy J1, Khaw KT3, Camargo CA Jr4.
... The Vitamin D Assessment Study is a randomized, double-blind, placebo-controlled trial that recruited participants mostly from family practices in Auckland, New Zealand, ... Participants were community-resident adults aged 50 to 84 years. ...
Oral vitamin D3 in an initial dose of 200 000 IU, followed a month later by monthly doses of 100 000 IU, or placebo for a median of 3.3 years (range, 2.5-4.2 years). ... A monthly 100 000-IU vitamin D dose was chosen because of pharmacokinetic evidence indicating that this maintains serum 25(OH)D levels above 35 ng/mL for a month after ingestion. ...
Of the 5108 participants included in the analysis, the mean (SD) age was 65.9 (8.3) years, 2969 (58.1%) were male, and 4253 (83.3%) were of European or other ethnicity, with the remainder being Polynesian or South Asian. Mean (SD) baseline deseasonalized 25(OH)D concentration was 26.5 (9.0) ng/mL, with 1270 participants (24.9%) being vitamin D deficient. In a random sample of 438 participants, the mean follow-up 25(OH)D level was [54.1 (SD 16.0) ng/mL = 134.78 nmol/L in vitamin D group vs. 26.4 (SD 11.6) = 65.89 nmol/L in placebo]. The primary outcome of CVD occurred in 303 participants (11.8%) in the vitamin D group and 293 participants (11.5%) in the placebo group, yielding an adjusted hazard ratio of 1.02 (95% CI, 0.87-1.20). Similar results were seen for participants with baseline vitamin D deficiency and for secondary outcomes [myocardial infarction, angina, heart failure, hypertension, arrhythmias, arteriosclerosis, stroke, and venous thrombosis].
Conclusions and Relevance:
Monthly high-dose vitamin D supplementation does not prevent CVD. This result does not support the use of monthly vitamin D supplementation for this purpose. The effects of daily or weekly dosing require further study.
PMID: 28384800 DOI:
Ingredient Dosage Frequency Administration See Below! As Appropriate serving(s) Daily No instructions provided.
What brand of ubiquinol do you use Michael? No love for Mitoq?
What brand of ubiquinol do you use Michael? No love for Mitoq?
I use any reputable brand: it's all Kaneka in the end.
No, no love for MitoQ. First, as I indicated, I'm taking it for physiological replacement, not some pharmacological mito antioxidant effect. Second, it would be foolish at this point to be taking it for some pharmacological mito antioxidant effect, since it's very clear at this point that it has none in normal mammals(1,2) — nor, indeed, is there any other evidence of any benefit in normal mammals, except maybe in skin cream.
References
1: Sakellariou GK, Pearson T, Lightfoot AP, Nye GA, Wells N, Giakoumaki II, Griffiths RD, McArdle A, Jackson MJ. Long-term administration of the mitochondria-targeted antioxidant mitoquinone mesylate fails to attenuate age-related oxidative damage or rescue the loss of muscle mass and function associated with aging of skeletal muscle. FASEB J. 2016 Nov;30(11):3771-3785. Epub 2016 Aug 22. PubMed PMID: 27550965; PubMed Central PMCID: PMC5067250.
2: Rodriguez-Cuenca S, Cochemé HM, Logan A, Abakumova I, Prime TA, Rose C, Vidal-Puig A, Smith AC, Rubinsztein DC, Fearnley IM, Jones BA, Pope S, Heales SJ, Lam BY, Neogi SG, McFarlane I, James AM, Smith RA, Murphy MP. Consequences of long-term oral administration of the mitochondria-targeted antioxidant MitoQ to wild-type mice. Free Radic Biol Med. 2010 Jan 1;48(1):161-72. doi: 10.1016/j.freeradbiomed.2009.10.039. Epub 2009 Oct 23. PubMed PMID: 19854266.
What causes the difference in safety between taking the 2 x 420mg PC vs 2 x 55mg citicholine? Would the two result in the same serum choline levels?
The diff' is that PC raises TMAO less than citicoline. I don't know which would raise serum choline more, but I prefer PC because it's both safer based on TMAO and I think consuming it this way is more conservative: my far-from-expert understanding is that CDP-choline is quite rare in the diet, being only present as an intermediate in PC synthesis in the CDP-choline pathway.
The diff' is that PC raises TMAO less than citicoline. I don't know which would raise serum choline more, but I prefer PC because it's both safer based on TMAO and I think consuming it this way is more conservative: my far-from-expert understanding is that CDP-choline is quite rare in the diet, being only present as an intermediate in PC synthesis in the CDP-choline pathway.
Do we know whether it raises TMAO less per total mg or per mg of choline supplied?
test
Why did you remove Lactoferrin, Inositol /IP-6 and Glycine from your regimen as per its previous version?
The diff' is that PC raises TMAO less than citicoline.
Do we know whether it raises TMAO less per total mg or per mg of choline supplied?
Per mole (properly) of choline supplied. We don't have actual quantification on citicoline, but it's been demonstrated that it raises it, and since citicoline is hydrolyzed in the intestine prior to absorption, the relative amount should be similar to that of choline salts; clean PC barely raises TMA(O) at all, whereas choline salts raise it ninefold.
In response to aribadabar's questions:
I quit IP6 because I have persistently high serum phosphorus (which is bad), and because my dietary IP6/phytate and inositol is already likely at the extreme end of the population (legumes and nuts). Additionally, there was little positive reason to take it, either: I don't have any history of kidney stones, I drink plenty of fluids and have a high-intrinsic-water diet, and no one has yet done a study showing it benefits otherwise-healthy aging rodents or humans. And if it's working by mobilizing NK cells, well, who knows what decades of incessant NK stimulation could do?
I quit the lactoferrin because I finally admitted to myself that there's never really been any good reason to take the stuff. And my iron stores are still right where I want them to be.
Glycine: I decided that I had to stop drinking water just before bed in order to avoid a mid-night trip to the bathroom, which seems like a more sensible way to ensure solid slip than doping myself up with supplements — and I'm reluctant to take it on an empty stomach. Plus, I suspect that it may have been the reason for my occasional bouts of waking up at 3 AM with a pounding heart and a sweat: my hypothesis is that this is due to Somogyi effect, arising from the interaction of glycine-induced insulin secretion with my having CR-associated high insulin sensitivity and low glycogen stores: see here and here. Certainly, I've had none of these episodes in the months since I quit taking it.
Michael, as followup on a discussion elsewhere, did you ever test serum retinol and RBP? Also would be interested in you 25(OH)D3, if you would be willing to share.
I've never seen any compelling case for RBP testing, granted my very large beta-carotene intake and small but nonzero retinol intake. My 25(OH)D3, as I mentioned, is now in the low end of the 30-40 ng/dL range.
Thanks. so this study: http://www.fasebj.or...23/4/1041.full doesn't concerns you?
Nope! I get ≈1/9 of the DRI RDA from retinol, and 5.68 times the DRI RDA for vitamin A as carotenoids from beta-carotene alone, plus lots of alpha-carotene: that more than coveres a genetic variation of up to -69% from the canonical SNP (and we don't know the percentage of slow-converters have been included in the studies used to set the DRI RDA: unless every single one of them had the reference SNP, -69% is a worst-case scenario). Plus, human and animal evidence shows that bioconversion is increased in the face of a high-fat diet (check), and is negatively correlated with BMI (covered).
It's just that I trust a cheap retinol and RBP test in my serum more than research in any other. Had these (fat-diet and BMI) also covered, but needed ridiculous high amounts just to normalize my levels.
But serum retinol and RBP don't seem to be reliable indicators of vitamin A status, and I have great night vision, no hyperkeratosis, and my immune system seems highly functional despite all the weirdness around CR immune function studies.
Michael,
"my iron stores are still right where I want them to be."
What levels e.g. of ferritin do you consider optimal for most people?
I like the entire suite of functional iron markers to be very low-normal. Absent such "full-spectrum" testing, low-normal ferritin.Michael,
"my iron stores are still right where I want them to be."[/size]
What levels e.g. of ferritin do you consider optimal for most people?
Hi Michael,
I'm curious as to why you don't take Rapamycin considering that at top of your post you state "whereas we now have extremely convincing evidence for rapamycin" as regards to supplements.
I'm thinking of getting my parents, who are in their seventies, on rapamycin (once weekly 5mg) + metformin as a stepping stone to the availability of senolytic treatments.
Thanks,
Chris
Because (a) rapamycin is really a pretty risky drug to take experimentally (at least at levels likely to be effective, assuming the rodent data does indeed translate — see discussion here and this followup) and (b) there seems to be surprisingly little advantage to starting rapa earlier in life vs. later, perhaps because its beneficial effects become more relevant in opposition to secondary aging processes or because the mixture of deleterious to beneficial effects shifts with the changing aging milieu — or perhaps simply because of changing pharmacokinetics, since in the mice at least plasma levels at a given dose are much higher in aged vs. young animals.
So I feel I've got some time, and we'll certainly know a lot more in a few years.
The stupidest thing in the universe is a life extensionist dead of the long-term toxic effects of his experimental fountain-of-youth pill.
Michael, there is a video on nutritionfacts.org which tells how our bodies can produce CoQ10 on our own (hint, you would have to eat green leafy vegetables and get some sun afterwards): https://nutritionfac...oq10-naturally/
On the Vit D, I looked into it a long time ago but the conclusion was that the study you reference was not legit (based on people taking in fish in Scandinavia or something, dont quite remember was a long time ago). The video had a different conclusion on that (3:12): https://nutritionfac...atural-levels/ This is why I personally take 10000IU on days without sun and 5000 IU on days with some sun in winter of few in summer.
This link states humans get in an average of a bit lower than 1mg of lithium a day up to about 3mg: https://getfit.jilli...thium-1831.html Vegetables and grains seem to be high in it.
Carninutrients: why do you take taurine and beta-alanine in such high doses? Taurine barely offers any benefits for as far as I´ve read and omnivores have an average intake of 100-400mg as I have read and about 50-300mg for beta alanine + 36,5% of b-alanine is carnosine so up to 822mg should be sufficient (sorry, no direct sources to back this up as I haven´t safed them but you can probably find the sources yourself).
Carnitine has been shown to not raise TMAO levels in vegans though: https://nutritionfac...ao-connection/
Plus, carnitine probably raises sperm quality (see the comments I made in the link; user: Leon)
B12 might be better in cyanocobalamin form as Michael Greger often suggests as there is more research to support it and the other forms don´t work for every person. It´s also the cheapest and safest form. Greger suggests 2500mg a week but if you look at this video, 3750 should be closer to the ideal dosage: https://nutritionfac...of-vitamin-b12/
Veganhealth.org has a page on choline and says the 450/550mg per day is based on a single old study. As user Darryl also pointed out, 170-300mg might be sufficient supplemented with betaine (easily obtained from wheat bran).
Zinc: wheat bran/germ offer insane high amounts of zinc. Pumpkin seeds and sesame seeds as well, but lower. Tryptophan can also be easily obtained from diet: http://nutritiondata...0000000000.html
Is there a specific reason you haven´t looked into spices and herbs? Ginkgo biloba might hold some promising effects for cognition and turmeric, sumac and cloves f.e. are very high in antioxidants. Amla (powder or berry/dried berry) and astaxanthin are also extremely high in antioxidants.
Too bad metformin, rapamycin and acarbose seem impossible to obtain. Any reason for not supplementing PQQ, NMN or c60? And why no n-acetyl glucosamine but sulphate/sulfate?
Michael, there is a video on nutritionfacts.org which tells how our bodies can produce CoQ10 on our own (hint, you would have to eat green leafy vegetables and get some sun afterwards): https://nutritionfac...oq10-naturally/
Greger is not a reliable source of health information. Does he provide direct evidence of this happening in vivo in aging mammals, or is this the usual mechanistic speculation based on in vitro nonsense? And if so, does he provide direct evidence that this happens in CR animals (as noted, that's why I'm taking it), or alternatively that it is sufficient to counteract the "normal" age-related decline?
IAC, sun exposure is a carcinogen. I'll take the pill. Ditto on vitamin D.
Too bad metformin, rapamycin and acarbose seem impossible to obtain.
They're only moderately difficult to obtain. Get a prescription or order from reliable online pharmacies.
And why no n-acetyl glucosamine but sulphate/sulfate?
The cited studies used GLS, not NAG.
On the Vit D, I looked into it a long time ago but the conclusion was that the study you reference was not legit (based on people taking in fish in Scandinavia or something, dont quite remember was a long time ago).
"something, dont quite remember was a long time ago" is not a good citation. IAC, this is a painstaking individual patient-data meta-analysis of eight independent prospective cohort studies from Norway, Germany, Iceland, Denmark, and the Netherlands, not some single study of "Scandinavians."
The video had a different conclusion on that (3:12): https://nutritionfac...atural-levels/ This is why I personally take 10000IU on days without sun and 5000 IU on days with some sun in winter of few in summer.
Greger is not a reliable source of health information. His argument here is based on a mixture of (a) older meta-analyses of studies on single outcomes and not individual patient-level data, and (b) the paleo-adaptationist fallacy that "natural" levels are better.
Carninutrients: why do you take taurine and beta-alanine in such high doses? Taurine barely offers any benefits for as far as I´ve read and omnivores have an average intake of 100-400mg as I have read and about 50-300mg for beta alanine + 36,5% of b-alanine is carnosine so up to 822mg should be sufficient (sorry, no direct sources to back this up as I haven´t safed them but you can probably find the sources yourself).
Taurine: see my paragraph on this, beginning "AjiPure Taurine: Absent in vegetarian diet;" and references (32) and (33) on benefits and dose. Beta-alanine: because those are the doses used in clinical trials.
No references, no argument.
Carnitine has been shown to not raise TMAO levels in vegans though: https://nutritionfac...ao-connection/
That's what's reported, yes — but (a) it's based on a single "carnitine challenge consisting of co-administration of 250 mg d3-(methyl)-carnitine and an 8-ounce sirloin steak" in a small sample size (n=23), and (b) presuming it's real, the reason why is presumably because carnitine is so low in the veg(etar)ian diet that bacteria that avidly metabolize it don't get the fuel they need to grow to substantial numbers in the gut. If you obviate that situation by taking a supplement every day, you'll be feeding those bugs and their numbers will expand accordingly, leading to omnivore-level TMAO production.
Plus, carnitine probably raises sperm quality (see the comments I made in the link; user: Leon)
Bonus! By not taking it, I get a little background birth control ![]() .
.
Veganhealth.org has a page on choline and says the 450/550mg per day is based on a single old study.
If it says that (link, don't claim), it's wrong: the DRI is supported by multiple studies, including those I cited in my linked "supplements for vegetarians" post.
As user Darryl also pointed out, 170-300mg might be sufficient supplemented with betaine (easily obtained from wheat bran).
Betaine raises TMAO. Wheat bran is not remotely a high enough source of betaine, and betaine not an adequate substitute for choline, to make up the gap.
Zinc: wheat bran/germ offer insane high amounts of zinc.
The bioavailability of Zn in wheat bran is extremely low. 2 T of wheat germ contains 1.8 mg Zn, 0.8 mg omega-6, and 121 mg of phosphorus, plus
Wheat Germ Agglutinin: no, thanks.
Pumpkin seeds and sesame seeds as well, but lower. Tryptophan can also be easily obtained from diet: http://nutritiondata...0000000000.html
Loaded with omega-6: no, thanks.
Is there a specific reason you haven´t looked into spices and herbs? Ginkgo biloba might hold some promising effects for cognition and turmeric, sumac and cloves f.e. are very high in antioxidants. Amla (powder or berry/dried berry) and astaxanthin are also extremely high in antioxidants.
Although a long-term prospective epidemiological study did find an association between Ginkgo use and slow cognitive decline, its power is limted by only requiring one reported intake at any of ten follwups assessments over the course of 20 yearas (1), whereas two well-done clinical trials (2,3) found no benefit. That's not a good reason for putting a concentrated phytochemical into your body for decades.
Antioxidants, shmantioxidants: that canard should have died in 1992. I'm not aware of any actual health benefits of any of these listed substances in normal, otherwise-healthy aging mammals after oral administration. Can you cite any (with primary scientific citations)?
Any reason for not supplementing PQQ, NMN or c60?
PQQ: I'm aware of no evidence of benefits in normal, otherwise-healthy aging mammals in vivo after oral administration. Can you cite any (with primary scientific citations)?
NMN: I'm taking NR; I don't think we know enough to think that either is better at this point, or that taking both is better than taking one at the same total molar dose. NR's supply chain is clearer, it has a monographed analytical method, and it's cheaper.
c60: a lot of hype over a badly-done, retracted animal study that doesn't pass the laugh test. There is at present no evidence of benefits in normal, otherwise-healthy aging mammals in vivo after oral administration — or can you cite any (with primary scientific citations)?
References
1: Amieva H, Meillon C, Helmer C, Barberger-Gateau P, Dartigues JF. Ginkgo biloba extract and long-term cognitive decline: a 20-year follow-up population-based study. PLoS One. 2013;8(1):e52755. doi: 10.1371/journal.pone.0052755. Epub 2013 Jan 11. PubMed PMID: 23326356; PubMed Central PMCID: PMC3543404.
2: van Dongen M, van Rossum E, Kessels A, Sielhorst H, Knipschild P. Ginkgo for elderly people with dementia and age-associated memory impairment: a randomized clinical trial. J Clin Epidemiol. 2003 Apr;56(4):367-76. PubMed PMID: 12767414.
3: Snitz BE, O'Meara ES, Carlson MC, Arnold AM, Ives DG, Rapp SR, Saxton J, Lopez OL, Dunn LO, Sink KM, DeKosky ST; Ginkgo Evaluation of Memory (GEM) Study Investigators. Ginkgo biloba for preventing cognitive decline in older adults: a randomized trial. JAMA. 2009 Dec 23;302(24):2663-70. doi: 10.1001/jama.2009.1913. PubMed PMID: 20040554; PubMed Central PMCID: PMC2832285.
Greger is not a reliable source of health information.
We will see in a short moment. Even though we started with CoQ10, let me first address vit D.
His argument here is based on a mixture of (a) older meta-analyses of studies on single outcomes and not individual patient-level data, and (b) the paleo-adaptationist fallacy that "natural" levels are better.
No, Greger actually said the opposite at 3:05; that the natural level actually is not the optimal level per se. So no ´paleo-adaptionist´ fallacy here.
"something, dont quite remember was a long time ago" is not a good citation. IAC, this is a painstaking individual patient-data meta-analysis of eight independent prospective cohort studies from Norway, Germany, Iceland, Denmark, and the Netherlands, not some single study of "Scandinavians."
I looked it up again, and let me summarize by giving a short chronogical history on vit D:
https://nutritionfac...recommendation/
First this video (from 2011) at about 1:01 shows about >80-90nmol/L is where your body will not be putting more vit D in circulation, about right in the middle where your conclusion of 75-100nmol/L is.
https://nutritionfac...vitamin-d-bate/. Then his conclusion here is 2000IU seems to be best for people in general. Off course, like you pointed out in your ´patient-level data´, the 2000IU is just an average. Some need more or less. You yourself take in about 500-1000IU, but you could be getting more sunlight than the people in Greger´s cited study did. Or you might be taking it in with your meals, which contributes to higher absorption.
However, this is a very old video of doctor Greger from December 2011. The same link also states an ideal of 80nmol/L at 1:27, which is what your study also cites.
Now is a more recent video from 2016. One of the statistics in this video looks remarkably similiar to the one you cited: https://nutritionfacts.org/video/how-much-vitamin-d-should-you-take/. However, this one is outdated. New data in this video shows about >135nmol/L is better than 80nmol/L. Why? Because some of these vit D studies are based on Scandinavian cod liver supplements, which contributed to increased mortality risk due to their vitamin A content, which was beyond the upper dosage. So the U-shaped curve is outdated.
Note the meta-analysis study you stated on vit D cites: ´European consortium of eight prospective studies, including seven general population cohorts´ So this study probably was from these cod liver studies were mostly from Scandinavian countries.
From here on I will just advise you to watch the entire video. After you´re done, we arrive at the video I linked earlier. Please watch this one again, and what I said earlier will make more sense now:
https://nutritionfacts.org/video/the-optimal-dose-of-vitamin-d-based-on-natural-levels/
I said 3:12 before, but I meant to say the study at 3:18. 5000IU pills make more sense now. Perhaps even 10000IU might be better on days without any sun. But it depends on several variables. For some 5000IU might be more than enough, or even 10000IU, just like Greger cited in some of his videos on vit D.
Now on CoQ10.
Does he provide direct evidence of this happening in vivo in aging mammals, or is this the usual mechanistic speculation based on in vitro nonsense? And if so, does he provide direct evidence that this happens in CR animals (as noted, that's why I'm taking it), or alternatively that it is sufficient to counteract the "normal" age-related decline?
Did you watch the video (entirely)? At 2:30 he shows a study which shows mammals can produce ATP themselves after consuming chlorophyll compounds. Or you can read the study yourself: https://www.ncbi.nlm.nih.gov/pubmed/24198392
And at 3:47 he shows a study which states our bodies can produce CoQ10 after sunlight exposure. Or view this study here yourself: https://www.ncbi.nlm.nih.gov/pubmed/22928808
Whether you´re doing CR or not, as long as you eat chlorophyll containing foods and expose your body to the sun, your body will produce CoQ10. I agree sun exposure is carcinogenic, that´s why I take vit D mself, but I guess some sun exposure is unavoidable right? Why not make good use of it? I couldnt figure out though how much was produced, but perhaps you could figure it out?
They're only moderately difficult to obtain. Get a prescription or order from reliable online pharmacies.
Also in the Netherlands? I looked online for any website but couldn´t find any.
Then on the carninutrients: I actually agreed with you. To be honest, I was pushing you a bit in order to get a response. I myself supplement with carninutrients as well for a few months now: beta-alanine, taurine, carnitine and creatine.
However, I did some research some time ago and found out carnitine, taurine and carnosine aren´t a problem in those who take in high amounts of protein every day (~.7g-.8g< protein per pound). Then our bodies would synthesize all we need. There are also some sources claiming our bodies can only synthesize up to 1g of creatine per day, when we need 2g total each day. But I am a bit sceptical of this, considering sites make very distinct claims about creatine and there being no site which accurately lists all creatine sources. It´s also pretty weird no amino acid except creatine would be a problem. I think it´s obvious why I think this is weird.
You do seems to be aware of the relationship between choline and TMAO. I haven´t looked into the choline studies you told about, will look into it. However, there is some evidence vegetarians aren´t getting enought carnitine either (when they take in only moderate amounts of protein, like 70-80 grams a day):
https://www.ncbi.nlm.nih.gov/pubmed/2756917; https://www.ncbi.nlm.nih.gov/pubmed/21753065;
Would you consider supplementing it now as well just like choline, even though there is a TMAO connection?:
https://nutritionfac...mao-connection/. I mean, carnitine should be as essential, just as choline after all.
I also have a little bit extra info about it in the following video, please read my comments: https://nutritionfac...in-supplements/
Loaded with omega-6: no, thanks.
Is there a specific reason you avoid omega 6? Omega 6 is only a problem if you eat it with omega 3, in which case the omega 3 gets ´behind in the line´ of what your body will use fas DHA/EPA. Just consume your omega 3´s first every day, then only omega 6 later. Or simply supplement with a sufficient DHA/EPA omega algae pill.
The bioavailability of Zn in wheat bran is extremely low. 2 T of wheat germ contains 1.8 mg Zn, 0.8 mg omega-6, and 121 mg of phosphorus, plus
Wheat Germ Agglutinin: no, thanks.
I said bran/germ as I was quick in my response, but the following links shows 100g wheat germ contains about 14-12mg, which is pretty significant: https://www.healthal...icles/zinc.php; http://nutritiondata...0000000-w.html. Toasted wheat germ even has 17mg.
And I don´t seed what´s wrong with lectins like WGA. They even have many benefits for our bodies: http://www.sciencedirect.com/science/article/pii/S0733521014000228. As far as I know, when lectins show negative effects, they either use high dosages or use unhealthy populations. Soy isovlavones don´t scare me for this reason, as gynaecomastia only was perceived in case studies involving at least a kilo of soy products daily.
The only one who seems to worry about agglutinin is Mercola, who is nothing more than a witch doctor in my eyes. He only wants to sell his products, unlike Greger who established a non-profit site where procedures goes towards charities.
Although a long-term prospective epidemiological study did find an association between Ginkgo use and slow cognitive decline, its power is limted by only requiring one reported intake at any of ten follwups assessments over the course of 20 yearas (1), whereas two well-done clinical trials (2,3) found no benefit. That's not a good reason for putting a concentrated phytochemical into your body for decades.
Well, never mind the ginkgo now. I just found out ginkgo should be avoided, read about what I typed here:
http://www.longecity.org/forum/topic/98805-known-negative-side-effects-on-certain-supplementsherbsspices/page-2#entry837103
But if a certain supplement is safe, I see no reason why long-term supplementation should be harmful. Whether it is a certain tea, herb, spice or regular food.
Antioxidants, shmantioxidants: that canard should have died in 1992. I'm not aware of any actual health benefits of any of these listed substances in normal, otherwise-healthy aging mammals after oral administration. Can you cite any (with primary scientific citations)?
Don´t have one at hand. But it´s handy for anti-aging and stress as far as I know. Here´s a handy startpage on it:
https://nutritionfacts.org/topics/antioxidants/
Never mind c60, PQQ and NMN, I decided I have no interest in them anymore. However, I do have a couple of questions for you I wandered about:
1) any reason why you´re vegetarian and not omnivorous or whole-food plant-based/vegan? When I looked at your diet I couldn´t spot any animal products though.
2) Are you aware of more people who list their diet and supplement regimen on this or another site in detail like yourself?
3) I need some help with niacin. RWhigham commented in this post something about niacin/niacinamide perhaps decreasing lifespan:
http://www.longecity.org/forum/topic/79920-nicotinamide-without-the-riboside-nicotinamide-by-itself-any-good/. Is this a typo?
And you yourself once said it Increases chance for diabetes. However, another post mentioned blood sugar is only raised temporarily. After same use this blood sugar rise will eventually disappear.
Is 500mg a sufficient dose or is 1g a lot better? I cant find any good info on it. Do take I´m only 24 years old, so I need less than someone older.
4) Ever thought about taking heart rate lowering supplements like valerian or adaptogens at moments of stress? Sure beats lavender, which has been associated with gynaecomastia (see my link about negative side effects linked earlier).
5) Any reason why you dont take spices like dill, chervil or cardamom?
6) Do you know anything about supplementing bromelain? Anything good or bad?
Final, are you one of the ´makers´ of this site? I gotta say I like the site and I thank you for it! :D
EDIT: here is your link about choline: https://www.crsociet...or-vegetarians/. And this is the one of veganhealth.org I was talking about: http://www.veganhealth.org/articles/choline. The article of veganhealth.org contains 5 of the 7 sources your link cites. It has 27 total sources however, also on a few other subjects. The two sources it doesn´t contain are xciv and xcv. I haven´t looked properly at it yet, but you might want to check it out yourself. It´s interesting to see however how they both arrive at different conclusions. Veganhealth.org doesn´t hold any bias, Jack Norris is more than happy to supplement when there is enought evidence to the contrary. He already supplements some nutrients.
I also just noticed you sometimes take 750mcg of melatonin. You can also eat an ounce of goji berries for about 15mcg of melatonin: https://nutritionfac...s-for-insomnia/. Because melatonin is potent it can increase blood levels 50-fold in the body, so one can get about 750mcg of melatonin per 1 ounce of goji berries.
I noticed Darryl has some info on phosphatidylcholine you might be interested in to read: https://nutritionfac...omething-fishy/
Michael, I have yet a few more questions: on k2, is there really a need to supplement it when one gets sufficient amounts of it (or k1) on a diet? Whether it´s mk7 or mk4? If so, what is the minimal required dosage? Especially for someone my age?
And regarding CR; is it also really making one live longer? So far I have read different evidence upon it on this site. Some say it has been shown to increase lifespan in animals, but not in humans. Perhaps it will only increase the quality of one´s phenotype?
But constantly CR´ing can´t be healthy right? If one does so he/she will continue to lose weight until he/she practically dies of starvation. My BMI is already most of the time in between 17.5-19.5, as of now it is about 17.5. I think I´m already CR´ing without me knowing it as I have lost some weight. You can´t encourage people to keep continue CR´ing until they become hospitalized?
And have you ever looked into coleus forskohlin for increasing BMD? It seems to be completely safe. DNA damage, cytotoxicity, general toxicity, liver damage and case studies all gave negative results. The only caveats I could fine is a study which noticed genotoxicity in Allium cepa (onions). It also raised heart rate 16% in a human study. But I´m not sure it´s a negative thing per se, as coffee also seems to raise heart rate, which you also take (though I´m not sure if decaf coffee raises heart rate). It might be a little bit undesirable when looking at it from a longevity perspective. But I´m not qualified enough to make this definitive conclusion. One study even noticed it being promising for cancer: http://onlinelibrary...320622/abstract
Michael, do you have any concerns about the long-term safety of glucosamine? Some say that there's a theoretical potential for kidney and eye damage.
Oral glucosamine increases expression of transforming growth factor β1 (TGFβ1) and connective tissue growth factor (CTGF) mRNA in rat cartilage and kidney: implications for human efficacy and toxicity.
https://www.ncbi.nlm...pubmed/21466783
Michael, do you have any concerns about the long-term safety of glucosamine? Some say that there's a theoretical potential for kidney and eye damage.
Oral glucosamine increases expression of transforming growth factor β1 (TGFβ1) and connective tissue growth factor (CTGF) mRNA in rat cartilage and kidney: implications for human efficacy and toxicity.
https://www.ncbi.nlm...pubmed/21466783
Hm. Your citation seems far too preliminary to raise concern (they don't even have protein levels in the kidney, and nothing in the eye); however, you triggered me to dig, and I see these two studies finding a rise in IOP with glucosamine. The second study, which is more robust in design, only finds a rise because of a mixture of a lower baseline (reversion to the mean?) and some post hoc fiddling, and "Although mean rise of IOP was statistically significant in the glucosamine group, more than 2 mm Hg rise in IOP was also more in the treatment group (34% of those receiving treatment vs 12.5% of patients on placebo)." And it was done in Iran.
However, even a suggestion of a risk may not be worth it to some people, especially if their inflammation is already low or they have reason to think they're at risk of glaucoma.
It'd sure be nice to have this done more robustly, and also to see some epidemiology on glucosamine supplement users.
Here's some more bad news about glucosamine: it has bad effects in both the normal and injured intervertebral discs of animal models, and at least in vitro, there are other problems associated with glucosamine.
Effects of Oral Glucosamine on Intervertebral Disc Matrix in an Animal Model
https://www.thespine...0776-0/abstract
Glucosamine supplementation demonstrates a negative effect on intervertebral disc matrix in an animal model of disc degeneration.
https://www.ncbi.nlm...pubmed/23324939
Glucosamine promotes longevity by mimicking a low-carb diet
https://www.longecit...-low-carb-diet/
Why not consume alcohol-free wine?
Full'a sugar, and several of the mechanisms for CVD protection from wine involve the alcohol.
IAC, I actually quit wine last October, after reconsideration of the epidemiology, particularly the nature of the observed stable low-level drinkers. Not going to detail that now ![]() .
.
Are you considering resuming glycine , perhaps earlier in the day given your possible somogyi effect, following this recent development @ the ITP: https://onlinelibrar...1111/acel.12953?
As for NR, are you considering suspending or adjusting the dose due to potential loss of methyl groups particularly at conventional doses - a hypothetical concern expressed here https://chrismasterj...amide-riboside/ ?
Some of your stack may partially offset this - e.g., creatine, choline - though not necessarily adequately. That was the short, anecdotal version of a more elaborate version presented in this podcast with Peter Attia: https://peterattiamd...hrismasterjohn/ at around 1:47:15
Hi Michael, not sure if you are still checking this thread but why not fisetin?
Are you considering resuming glycine , perhaps earlier in the day given your possible somogyi effect, following this recent development @ the ITP: https://onlinelibrar...1111/acel.12953?
The dose used in the ITP study was quite large (8% of diet by weight), was initiated in young adulthood (9 mo), and the effect on lifespan quite modest and uneven (the 6.2% median and 4.5% max figure is averaged over 3 sites, with a much larger effect at UTexas dominating negligible effects in the other two labs); that's not attractive enough for me to consider such a dramatic supplementation program.
As for NR, are you considering suspending or adjusting the dose due to potential loss of methyl groups particularly at conventional doses - a hypothetical concern expressed here https://chrismasterj...amide-riboside/ ?
Some of your stack may partially offset this - e.g., creatine, choline - though not necessarily adequately. That was the short, anecdotal version of a more elaborate version presented in this podcast with Peter Attia: https://peterattiamd...hrismasterjohn/ at around 1:47:15
I'm actually currently taking only 125 mg of NR or NMN 4 d/week, with 250 mg NR 2 d/wk and a one-day weekly holiday, and as you say I have partially offset this potential concern (plus an extremely high dietary intake of folate). I do think it's important to have a decent level of methylating nutrients. I've noted the potential problems of methylnicotinamide, and it's not clear whether/how much that's due to MeNAM being itself toxic vs. it depleting methylating units.
Hi Michael, not sure if you are still checking this thread but why not fisetin?
if you have started , what is your protocol ?
I'm not, yet, though I'm certainly considering it and have almost pulled the trigger more than once. Animals on CR per se accumulate fewer senescent cells as they age (PMIDs 26983960, 20844316, 29575469) — including, apparently, CR humans (PMID 29575469 ) — so my risk:benefit is more favorable than for most. Additionally, the results of a senescent cell ablation study by Dmitry Bulavin at Undoing Aging (I hope video will be up soon) scared the snot out of me; I am awaiting to read the paper and understand more before adopting any senolytic protocol (though fisetin, specifically, seems to be less hepatotoxic than other senolytics, and liver damage was the site of the horror in the Bulavin study).
As to protocol: most people are defaulting to the Mayo Clinic's study protocol of 20 mg/kg/day, orally for 2 consecutive days (often with some effort to enhance bioavailability). The dose seems about right or a little bit high based on either the HED method or true allometric scaling, but on reflection the time period does not: in the rodents, the acute clearance protocol was 5 days, and if anything the idea of "biological time" might suggest a longer period for a longer-lived mammal.
Why split up the lysine within and outside of meals? Or was this exclusively to keep levels high ( steady levels pertinent t to lysine supplementation for prevention of encapsulated viruses? Instructions state take on empty stomach to prevent amino acid competition for absorption, is this to hedge your bets?
I can understand the desire for reliable contaminant-free products such as AgiPure lysine and taurine given your experience with creatinine. Do you equally trust any other source? I am contemplating 1000 mg rather than 500 mg capsules of these if possible - and staying away from the powders - and it would be more convenient to take one 1000 mg pill than two 500 mg pills. Woild pure encapsulations, Thorne or other manufacturers ensure fidelity of the product equally if they are NSF verified or do you use other criteria?
Also, I see that you understandably prefer Glucosamine sulphate over glucosamine hydrochloride. What brands do you recommend to source it?
Lysine timing: yes, it's to keep levels up. Not sure what you're asking about "hedging my bets" on lysine: I don't want it competing with other aminos (currently only Trp) for passage of the BBB.
Brands: First, AjiPure is a branded raw material: Thorne and Pure Encapsulations are brands of finished consumer products. I just don't know enough about teh QC of particular retail brands or what they should even be looking for (or whether they'd be looking for it). IT took quite some time for researchers to even identify all the the possible contaminants in Showa Denko's tryptophan that might have been responsible for the EMS crisis, and we still don't know which is the actual culprits decades after the fact. How would one even know where to start on lysine or taurine?
Any reputable brand of GLS should be fine, AFAIK.
Thank you for clarifying on raw material vs brand. Sound advice on selection.
At a micro-level, I check with ConsumerLabs, but they don't always have an up-to-date listing for any given supplement. A variety are available from Amazon.com, but presumably this a poor screen!
From your years experience in the industry, what criteria do you use to vet "reputable brand?' Do you have a short list of acceptable sources?
From your years experience in the industry, what criteria do you use to vet "reputable brand?' Do you have a short list of acceptable sources?
Criteria would include having been around for a while; showing scientific literacy and modesty in their marketing materials; have passed some third-party testing (CL, Labdoor, Consumer Reports, occasional media exposés, etc); having their GMPs certified by UL, USP, or NSF; being willing to share third-party certificates of analysis; having easily-found US/Canada/EU address and contact information, and being responsive to inquiries; not having FDA Warning Letters (like this) against them; having non-deceptive Supplement Facts and related info (like not playing fast-and-loose with serving sizes or elemental values); and even having professional-looking labels and packaging (if they can't even invest in a decent label, how can they run a clean production facility?).
I'm not saying they should tick all of these boxes, but those are all things I look at and consider valuable.
That's a great list. Some are straightforward such as UL / USP / NSF certification. Others compel investigation, such as sharing third-party certificates, and yet others are have subjective as well as objective information such as responsiveness to inquiries, transparency, etc. This last category is easiest to assess based on past experiences. Do you feel comfortable naming the brands you felt passed the last and presumably also other criteria? Reliability and quality may be a moving target, but starting with those "so far, so good" companies would not be a bad start.
I have "graduated" assessing you full list and have incorporated several new supplements thanks to your post with only modest departures. At this point, my next step is evaluating alternative regiments and possible additions.
For your glycine ( I know you are not using this one), lysine, and taurine, would you feel comfortable with taking 1000+ mg at a time rather than 500 divided from a safety and tolerance perspective? As you alluded to, you divide primarily for either greater absorption, or to spread out the serum levels so that it can be more biovailable more of the time. In drawing my own health optimization versus convenience regiment I am entertaining taking daily, in the 1000-2000 mg range recognizing this may be less effective than your carefully cultivated regimen; are there liabilities I may be overseeing besides and accepting the efficacy vs convenience tradeoff?
On the subject of possible additions, in a non-diabetic without hyperlipidemia, do you see any benefit for berberine. I read your comments about metformin above and realize it has never as unitherapy yielded good evidence for life-extension ( indeed, quite the oppososite). However despite the overlap with AMPK mechanism of action with metformin, berberine may also act as a PCSK9 inhibitor. There is an additional question of bioavailability, though it least some formulations are purported to have greater nonavailability [ https://onlinelibrar...0.1002/ptr.6282 ], and berberine has additional potential albeit theoretical benefits including as Darryl recently pointed out in another thread systemic rather than strictly hepatic circulation as is the case for metformin. As for the PCSK9 inhibition, anecdotally Peter Attia in an interview recently related his clinical experience that high PCSK9 producers tend to see their LDL go down by about 20% when used for this purpose - Incidentally, what is your take on Attia in the longevity space? IAC, aside from PCSK9, berberine influences nutrient sensing in other potentially beneficial ways [ https://www.ncbi.nlm...les/PMC5839379/ ], which if low-risk may perhaps justify a lower threshold to supplement despite less-than-convincing outcomes assessments thus far.
You have not stated your lipid profile, but even on the last point alone, why not lower your LDL further, the the evidence from PCSK9 inhibitors (e.g., the from the FOURIER trial), with evidence getting the LDL is low as <=30 potentially yielded benefit. While metformin has its own inconveniences in and intolerances ( lower the anerobic lactic acid threshold with possible fatigue and GI intolerance), it seems at first glance PCSK9 may be a lower risk addition to your regimen. Or are your concerns over genotoxicity or other matters greater than that expressed by others at a clinical dose of say 1000 mg twice daily - your thoughts?
And would you hesitate to take both a metformin and PCSK9 together or might the double AMPK mechanism of action be beneficially synergistic without too much concern about deleterious synergy?
Finally, if applicable, if you did select a berberine supplement at some point, which formulation and brand would you trust most for fidelity and bypassing the first pass effect?.
Footnote: off-topic but germane to correspondence, I noticed that you cite your references. What citation manager do you use? And how do you cite passages - indented and with a vertical line indicating taken from elsewhere - from paragraphs taken from other parts of the internet outside of the current Longecity thread? I find the quoting mechanism self-explanatory for Longecity proper, not not so if I am looking to insert a passage from other parts of the internet.
Feel free to PM me directing me to the best help file, etc, if that helps. I aim to improve the quality of my posts.
Hmmm, I can't seem to edit my post successfully with it saving the changes. Wanted to add this interesting summary regarding its positioning in nutrient sensing pathways ( see: https://www.ncbi.nlm...les/PMC5839379/ )- I know you are not generally very convinced nor am I without strong long-term observational data with quality trials at leaset in model organisms if not people..... however, if ( a big if depending on your response) it is deemed low risk as a supplement dosing, might thislower the threshold to supplement with its interesting mechanistic and some albeit not ideal supportive clinical data at this point?
Also, since I mentioned him, would be interested in your take on Dr. Attia. I don't know much about him but he seems to be increasingly positioning himself in the translational longevity space. He and Dr. Rhonda Patrick seem to be brining to the mainstream some ideas formerly restricted more narrowly to Longecity and the broader LE grassroots and research communities.
At this point, my next step is evaluating alternative regiments and possible additions.
You mean "regimen," not "regiment" ![]() . I am amazed by how many people make this error: there's a whole regiment of them on Longecity alone.
. I am amazed by how many people make this error: there's a whole regiment of them on Longecity alone.
For your glycine ( I know you are not using this one), lysine, and taurine, would you feel comfortable with taking 1000+ mg at a time rather than 500 divided from a safety and tolerance perspective? As you alluded to, you divide primarily for either greater absorption, or to spread out the serum levels so that it can be more biovailable more of the time. In drawing my own health optimization versus convenience regiment I am entertaining taking daily, in the 1000-2000 mg range recognizing this may be less effective than your carefully cultivated regimen; are there liabilities I may be overseeing besides and accepting the efficacy vs convenience tradeoff?
It might be fine with taurine, but the timing of glycine (either for sleep or life extension) and lysine are specific to their use, and are to maintain continuous serum exposure, not to increase bioavailability AUC: see the discussion in the post.
On the subject of possible additions, in a non-diabetic without hyperlipidemia, do you see any benefit for berberine.
I've seen far too little long-term human or animal data on either safety or efficacy. I'm not at all convinced by the limited animal evidence that it even is a PCSK9 inhibitor, even in rodents — and if it is, if the effect is durable, since if it happens at all it happens at the transcription regulatory level, which could very well gradually fade due to feedback systems. Moreover, lat time I looked, all the human trials with LDL-C outcomes that have been done in nondiabetics (which is the relevant study design for a PCSK9 inhibitor) have not only been small and short-term, but have used combinations with red yeast rice and often many other ingredients, so one doesn't know what if any contribution the berberine is making — or, again, if it's durable.
And would you hesitate to take both a metformin and PCSK9 together or might the double AMPK mechanism of action be beneficially synergistic without too much concern about deleterious synergy?
I focus on empirical outcomes, not mechanisms, and I'm not impressed that AMPK is a good target to focus on even granted that; nor am I convinced that it's a particularly important mediator for either metformin or berberine. And if it were, and we were to wallow in mechanistic speculation on the question: usually when you get an effect of 2 different agents that work through the same mechanism, it's more likely that you get a sub-additive effect than a synergistic or even additive one, unless one of them comes at it both potently and upstream rather than directly: there's only so far one can push these things holding genetics and lifestyle constant.
I noticed that you cite your references. What citation manager do you use?
I don't use one.
Also, since I mentioned him, would be interested in your take on Dr. Attia. I don't know much about him but he seems to be increasingly positioning himself in the translational longevity space. He and Dr. Rhonda Patrick seem to be brining to the mainstream some ideas formerly restricted more narrowly to Longecity and the broader LE grassroots and research communities.
I'm impressed by Dr. Attia — not so much for his knowledge (which is extensive) or his views (with which I not infrequently disagree), but for his self-enforced intellectual humility (he admits that this is effort for him, his default tendency being toward overzealous confidence in his views), his data-driven approach, and agnosticism. I get thie impression that he has evolved on these issues quite significantly as a result of his experiences at NuSi and the drivers of his departure from same. He has his frameworks and preferred hypotheses but is decidedly nondogmatic about them, and doesn't try to force the data on an individual patient into them when they clearly don't fit (viz. his arguments with people who insist that they can ignore a sky-high LDL-P so long as it's the result of a ketogenic diet, their CRP is low, and they don't have any coronary calcium). He also has great guests on his podcast, and can glean a lot of value from what would seem to be an unpromising guest.
By contrast, while Patrick also often has good guests, she has the unfortunate tendency of stating preliminary hypotheses as facts, and equally of a kind of intellectual passive-aggressiveness; she also fails to take in the key heuristic captured in the Attiaism "That's a fact, but is it a reason?" This last point is well illustrated in the lengthy exchange that Attia and Patrick have in her podcast "Peter Attia, M.D. on Macronutrient Thresholds for Longevity" etc, starting around 25:33 (in the transcript, beginning at "I like to think about it at the level of the gut" etc).
Hi Michael,
Your comments were again valuable.
Please keep any corrections coming - though I know the difference ( autocorrect at work?), and noticed the systematic error in the posting, I could not edit it out with attempts to edit unsaved. Hence the two posts back-to-back. Personally my pet peeve - is loose vs lose!
So you type references by hand every time, in full, numbers and all, or is there a part of PubMed or your favorite search engine where the full citation is appropriately formatted in full? For example if you are citing https://www.ncbi.nlm...les/PMC5715805/ , do you click on "Citation" on the upper right and then select "AMA Format" or do you have another method? I have published lengthy manuscripts offline using citation managers embedded within my word processor, but have not thus far for web-forum posts which I admittedly type on the fly bypassing the word processor. Perhaps I should reconsider my practices for quality control considerations.
I agree with your comments regarding Attia, and thought the link illustrated it well. I do enjoy them both, though Patrick admittedly seems at time prone to over-excitement and consequently asymmetric presentation and endorsement of a particular pet subject ( say NRF2 enhancers, broccoli sprouts, and Sauna therapy). It would be great to have more of a synthesis with contradictory findings or something akin to AUB's "contrary/null findings" https://shockcenter.uab.edu/ To her credit though she does a much better job than 99.9% of the healthspan sphere trying to present data in perspective, and they both also share a higher degree of transparency, minimization of conflict of interest, and interest in scientific integrity which is sadly uncommon in this space.
I share many Attia's "obsessions" and philosophy of "strong convictions, loosely held," esp. "loosely held," and like Attia I find that as my absolute knowledge in longevity science expands my perception of my relative knowledge diminishes precipitously ![]() This is humbling but motivates me to dig deeper.
This is humbling but motivates me to dig deeper.
Regarding "the timing of glycine (either for sleep or life extension) and lysine are specific to their use, and are to maintain continuous serum exposure, not to increase bioavailability AUC," possibly for lysine, and certainly for glycine ( which you are not presently taking), I am curious how the pharmacokinetics and pharmacodynamics might be influenced by meals.
That is, while spacing out the glycine regularly may keep the serum exposure more uniform, could some benefits of glycine supplementation be in relative to that of other serum amino acid levels at the time of intake? If so, this would be influenced by intake relative to meals-
To be concrete, if I take all my glycine during a single daily meal, I would certainly would absorb less glycine by competitive inhibition via other dietary amino acids, however I can presumably compensate for this by increasing the glycine dose taken with that daily meal. On the other hand, the glycine that I do take that meal may have the advantage of contributing to less absorption of methionine and/or the nutrient sensing sequela of said methionine, by maintaining higher hepatic glycine levels.
@ Michael: I find your general approach and evidence based regimen rather useful. Given the amount of expertise you put into your supplement regimen just one question. As a little side-obsession on my part I have read a little bit of the Glucosamine literature. Therefore, could you explain in a little more detail the rationale behind the 1500 mg per day dose?
It's the most commonly used dose in people using it as a joint-support supplement. So it ended up being the most common dose in cohort studies done in humans. Though it never had any particular basis even for joint support when established by rather less-scientific supplement companies/natural health remedies decades ago.
The studies done in rodents indicate (if translatable to humans), that somewhere above 3 mg/day might lead to better life extension. The mice-lifespan-study used the people-equivalent of 5-7 g per day. In human cohort studies the most frequent intake/same intake for lower body mass - that is, a higher dose - generally lead to better outcomes. Also the side effects appear to be very limited compared to life-extension drugs such as metformin or rapamycin (human data).
It could be argued, that people can't get the mice-benefits of rapamycin, as they are unable to sustain the side effects of mice-equivalent administration. The same can't be said for glucosamine. So.... why do you see 1,5 g as more justified over 3 g or even 6 g ?
On that on glucosamine, have you found any supplements in the sulfate formulation that are 1500 mg per tablet?
I have only found up to 1000 mg per tablet in the glucosamine sulfate form ( pure encapsulations). If you know a brand, please share.
could you explain in a little more detail the rationale behind the 1500 mg per day dose?
It's the most commonly used dose in people using it as a joint-support supplement. So it ended up being the most common dose in cohort studies done in humans.
Yes ... exactly.
The mice-lifespan-study used the people-equivalent of 5-7 g per day.
I assume you're deriving this from the FDA HED calculation. Showing our math, in PMID 24714520, , the mice consumed ≈4 g of chow per day (Fig. 4a and Supplementary Fig. 2a,b), which contained 10 g/kg glucosamine), and weighed ≈33 g (Fig. 4d and Supplementary Fig. 2g–h). So that's [(.004 kg chow x {10,000 mg GLN/kg chow})/.033 kg body weight) ≈ 1212 mg GLN/kg mouse. Per HED, this is 98 mg/kg human = 6879 mg for a 70 kg human.
OTOH, per direct allometric scaling, it's even larger: 12502 mg!
It's important to remember that these methods of calculating human-equivalent doses are necessarily only very rough-and-ready: they can't account for any of the many ways that model organisms' metabolisms vary from ours — just the sheer metabolic rate. By contrast, 1500 mg is a human dose that's been wisely tested in clinical trials and used in the community for decades, that seems sufficient to have clinical effects and that the epidemiology suggests lowers mortality — and in this case, not likely because of healthy user bias, since people take GLS to relieve arthritis symptoms (and often other joint problems), and not because they're health-conscious.
On the other hand:
Also the side effects appear to be very limited compared to life-extension drugs such as metformin or rapamycin (human data).
I'd agree with you that glucosamine certainly seems safe, though I think we need to keep an eye (pun intended) on the possible IOP effect noted by Florian, above. More recently PMID 31104873 reported out "Effect of glucosamine sulfate on intraocular pressure in patients with knee osteoarthritis: A prospective randomized controlled trial," an open trial of 42 subjects finding "no differences in the IOPs between the groups (P>0.05) nor differences in baseline IOPs within each group compared with each follow-up visit (P>0.05)" between subjects receiving "1500mg of crystalline glucosamine sulfate once daily for 6 months [vs. controls]... at 6 weeks, 3 months, 6 months, and 9 months," which is a larger trial than the previous reports, but it's still small, was unblinded (ha ha), and was carried out in Thailand, where standards may not be as good. I'd also like to know the role of any sponsor in the trial, which isn't disclosed in the abstract and unfortunately I've not been able to acquire the full text.
Metformin is an extremely benign drug, although metformin is useless for life extension.
Certainly the side-effects of rapa are very serious and should be treated as such (though it bears remembering that the reported side-effects are from patients in very bad medical condition to begin with, and may not be as serious in otherwise-healthy aging people taking the same dose). OTOH, there is also a hell of a lot more data supporting its anti-aging effect than the single rodent study for GLS (and that, with no numbers, and a somewhat unclear, seemingly gender-specific, and unquantified effect on maximum lifespan).
Though it never had any particular basis even for joint support when established by rather less-scientific supplement companies/natural health remedies decades ago.
What is your basis for saying this?
The studies done in rodents indicate (if translatable to humans), that somewhere above 3 mg/day might lead to better life extension.
3 mg daily? I assume you mean 3 grams — yes? And where does this number come from?
In human cohort studies the most frequent intake/same intake for lower body mass - that is, a higher dose - generally lead to better outcomes.
What is your evidence for this?
It could be argued, that people can't get the mice-benefits of rapamycin, as they are unable to sustain the side effects of mice-equivalent administration.
Certainly it seems likely that the effective dose for life extension with rapamycin will be lot higher than the 5 mg once a week being widely adopted on the basis of Alan Green's say-so. I see you agree, albeit that I think you may overstate your case somewhat. But we don't really know if the side-effects are tolerable as there are so few cases of people even trying.
On that on glucosamine, have you found any supplements in the sulfate formulation that are 1500 mg per tablet?
No, but I haven't looked: I avoid tablets in favor of capsules where possible because they're so often screwed up (turned into little insoluble pebbles), and 1000 mg tablets would likely be difficult to swallow.
My error on the ubiquinol: I take 50 mg. This is probably leftover typing from when I was taking 10 mg of ubiquinone ("regular" CoQ10).
I notice your productive attempt to punch some holes into my GS-obsession, so let's get started ![]()
Obviously any translation from animal data is to some degree speculation. Allometric scaling for drugs tries to take account of different metabolic rates, but there is scant knowledge of differences in clearing of individual supplements by mice-detoxification mechanisms vs. humans - let alone if the supplement is even effective in humans. Nonetheless: as long as there is no better method available and lacking life-extension RCTs for humans, scaling the mice-data at the moment is the best life-extension data. Obviously useless if we wouldn't also have good reasons to assume, that the GS is effective in humans.
In respect to translating the mice data, the evidence is actually better than for Rapamycin. As you wrote before: total mortality for humans taking GS was quite notably reduced in a large-scale prospective cohort study in none-pathological people. We lack similar data for Rapa in humans... taking Rapa is based on the assumption, that the mTOR-connection is highly preserved and thus the life-extension effects seen in short lived animals (notwithstanding the question of not using allometric scaling for people taking it for LE).
Basis for the history of GS: Google
It's somewhat scattered over the internet, but you may start with one of those summarizing sources and their references
https://www.ncbi.nlm...les/PMC1120508/
https://www.ncbi.nlm...pubmed/15846645
https://www.thelance...0040-5/fulltext
long story short: based on some crude conclusions (glucosamine and chondroitine are part of cartilage... so taking it should improve cartilage) some veterinarians began first injecting it in animals; getting mixed results. A lack of good alternatives for osteoarthritis in humans and the compelling argument laid out before ("it's part of cartilage, so eating it improves cartilage") some pharma/supplement-companies began marketing different versions of GS for human consumption in the 90s. Despite no compelling results from studies, heavy publication bias and no good rationale for 1500 mg.
Yes. You are right. It's 3 g. Not 3 mg. It was a typo. I apologize for that and promise to be more careful in the future. I hope no one did assume, that I was jumping from 1500 mg to 3 mg.
Base: some inference based on the mice-autophagy paper:
https://www.ncbi.nlm...les/PMC3772083/
3 g per day was the mice equivalent administered to achieve the AP results, "beating" the human equivalent of a multi-day fast. This assumes that AP is a major driver of the effects of GS (which I personally find plausible, given GS apparent effect on cancer). The 3 g were injected though.
Better outcomes in humans: in some analysis of the vital data, participants reporting a higher intake of GS had (much) better cancer-results than low- and non-users:
https://www.ncbi.nlm...les/PMC3671752/
https://www.ncbi.nlm...les/PMC3175750/
As circumstantial evidence from the nurse-health-professional-study, people taking GS with normal BMI had much better results than overweight participants (after correcting for confounders):
https://www.ncbi.nlm...nihms799160.pdf
To be clear: if this would be Rapamycin I would be cautious about "overdosing" (aka going above the arbitrary 1,5g established by lack of evidence in the 90s). Side effects might occure not noted on lower dosis and U-shaped mortality curve is bound to set in at some point. But mega-dosing GS in rodents for up to a year lead to no notable side-effects in rodents. There doesn't appear an LD50 for rodents at very high doses either:
https://mafiadoc.com...bc5223bd8f.html
(note: this review actually reports LD50, while the original papers cited just state, that the LD50 must be somewhere above the maximum dose used in the studies).
And at least one-time mega-dosing GS in humans - that is injecting 30 g in one sitting - is well tolerated.
Now I'm not saying humans should inject 30 g of GS per day (which certainly requires a much higher oral intake, given the leveling-off of the bioavailability curve). But given how surprisingly harmless GS appears to be - even compared to metformin - I find it justified to get more in line of the mouse-lifespan-study. So more than 1,5 g/day.
Your take?
as a further data-point for dose-depended effects, there is an in-vitro study, that demonstrates increasing downregulation of activation of mTor in a dose-dependent manner and upregulated AP in turn:
https://www.ncbi.nlm...les/PMC5983587/
That of course doesn't tell us, if the concentrations used are physiological - or if mTor is the major driver of autophagy in GS. At least one study conducted an experiment showing that GS still induces (increased) AP if mTor is silent:
https://www.scienced...025522?via=ihub
however, that increased AP is the major driver seems to become more and more clear:
https://www.jstage.j.../_html/-char/en
and as the mice-AP-paper demonstrates, GS is able to increase AP quite dramatically at physiologically achievable levels (much more than fasting by volume of AP-vesicles). In addition mitophagy (targeting damaged Mitos) seems to be up-regulated as well.
Therefore, given that both mice-paper (the life-span and the AP-paper) use doses that are closer to 6 g of oral intake per day; given that at least in the vital-data you can deduce a clear dose-dependent effect; and given the dose dependent inhibition of mTor by GS + especially the safety of GS.... could it be worth the risk, to take 3 g or 6 g per day? Or is it by Bayesian logic not also "risky" not to take more than 1,5 g - given the evidence so far?
Why not take glucosamine along with chondroitin? An analysis of the NHS and HPFS studies claims that glucosamine + chondroitin reduces CRC risk but not glucosamine without chondroitin.
Use of glucosamine and chondroitin supplements in relation to risk of colorectal cancer: Results from the Nurses' Health Study and Health Professionals follow-up study.
I'd be happy to discuss the pros and cons on the main forum (let's reserve this space for Michael's stack); in short possible cons in comparison to GS:
- greater lack of data for safety
- chondroitin is almost exclusively studied in combination with GS, which makes is hard to impossible to assess its effect
- lower bioavailability in trials
- several times higher price gram for gram
- unclear mechanism of action on cellular level
saying this: chondroitin might turn out to be a good idea. But the quality and scale of evidence is considerably below GS.
Why not acarbose? As you noted "pretty promising results for acarbose as well." It well-established in diabetics management and without the same concern for immunosuppression/glucose tolerance/hypercholesterolemia, etc. as purported with rapamycin..
Side effects appear mostly limited to GI intolerance.
On that note, on allometric considerations:
A 0.02 kg mouse, on a "medium" dose of 1000 mg/kg (ppm) [ https://onlinelibrar...1111/acel.12898 ], the 20 mg dose comes to - for a 55 kg human - [ 0.75 exponent : http://clymer.alterv.../allometry.html ] about 7595 mg.
This is a lot more than 100 mg/meal ( or 300 mg/day ) maximum for acarbose. Is your concern that 100 mg / meal does not reproduce the effect?
OTOH, half life and metabolic rate considerations may not be an issue at all since the MOA is simply alpha glucosidase inhibition before it gets eliminated unchanged, Further, it appears the prescribed doses for diabetes blunt/ameliorate glucose spike to the extent that this is suspected ( along with microbiome alteration) a major posited mechanism of action: https://www.youtube....h?v=Jvj4Ba5E7GM
Do you have any concern regarding stimulating mTORC1 from the periodic lysine you take at those doses?
While lysine does not invoke the same degree of stimulation on mTORC1 as, say, leucine, arginine, and glutamine, its contribution to mTORC1 stimulation above a threshold is nontrivial:
- https://www.ncbi.nlm...pubmed/24474444
- https://www.ncbi.nlm...pubmed/26366928
- https://www.ncbi.nlm...pubmed/30184226
Certainly, it has been argued that "While addition of lysine and/or methionine have been shown to increase phosphorylation of rpS6 and Akt in the muscle under certain conditions, these results are typically observed during periods of protein deficiency, or in in vitro studies" Source: https://onlinelibrar....1111/jpn.12992 ).
However your practice of CR - along with your practice of protein moderation - likely positions your insulin/igf-1 signaling (iis) pathway phenotypically with overlap with such a "low protein" model, given the substantial documented crosstalk between these nutrient sensing pathways.
Moreover, that study was in aged horses , and the other studies I cited are consistent with nontrivial increased mTORC signaling with lysine supplementation - the real question, I imagine is whether the degree of activation via modest supplementation is clinically significant if one goal it to keep MTORC signaling on the low side.
You're not getting 800 mg piracetam.
Taurine might allow more lithium to accumulate in the body. Is this a cause for concern even with low-dose lithium? Would the lithium dose need to be adjusted?
I'm not that worried about side effects, but I am worried that the possible beneficial effects of around 1 mg of lithium might be eliminated if it is allowed to accumulate too much.


















































Here the intervention group was only a small amount over outright deficiency, and the intervention group was quite high, but there was no effect at all on any cardiovascular outcome; there wasn't even an effect when looking at subjects who started the trial in outright deficiency. They have a point that daily dosing might be better than once-monthly bolus, but that's a pretty slim thread.
These results support prior work by Autier et al (PMID 24622671) showing pretty convincingly that the apparent benefits of high 25(OH)D levels are due to reverse causation: inflammation and a variety of undiagnosed early-stage disease processes lower one's vitamin D levels, so having high vitamin D becomes associated with good health, when it's ill-health driving low D rather than high D driving good health.
At 1000-1200 IU/d, I have consistently had a little over 40 ng/dL serum 25(OH)D3. I've been tapering back for years now to reach the low end of the 30-40 ng/dL range, and at 500 IU/d I am now finally fairly steadily there when measured in what passes for winter in these parts.
AjiPure Taurine: Absent in vegetarian diet; significant, altho' not ideal, data that it reduces the risk of CVD and other mortality.(33) NB that the EPA/DHA and taurine content of fish and seafood are major confounders to drawing inferences about observed benefits of fish consumption in epidemiological studies; while there are controlled trials showing lower risk of a second heart attack or major cardiovascular events with EPA/DHA supplements or extra ALA, there is as yet no real equivalent with taurine. In in Japan, the average intake appears to be 225 mg/d in males and 162 in females, with the highest intakes >1000 mg.(34) Additionally, recent studies have found that some of the endocrinological and "resillience" effects of CR involve the cellular generation of H2S via the transsulfuration pathway;(56-59) and a recent clinical trial(60) not only confirmed a previously-reported hypotensive effect of taurine, but showed that it elevates circulating H2S, and (in rodents) did so by elevating protein expression of the two key enzymes in the transsulfuration pathway.
Rite Aid B-Complex With B12: Rite Aid: who'd'a thunk it?? I've been looking for a supplement like this for years! Provides RDA-ish levels of all B-vitamins, except that it contains no folic acid. I get a ridiculous amount of folate in my diet, I have no MTHFR reductase mutations, and if one does think one needs a supplement (after having first tried just increasing one's intake of green leafy vegetables), one should err on the safe side by avoiding folic acid in favor of L-5-methyltetrahydrofolate. I started taking this in order to more conveniently cover my B12 needs, and in hopes that it plus the small amount of B6 would lower my Hcy. I needed larger-caliber weapons (see above), but continue to take it.
Melatonin: for sleep when stressed, wide awake, or jetlagged. 300 mcg is sufficient to raise levels to normal physiological youthful ones and apparently works as well as higher doses ((22,23), and see (21)) and doesn't produce the 'hangover' sleepiness sometimes seen with the supraphysiological 3 mg (and up) doses that became ubiquitous thanks to the recommendation of the once-notorious Melatonin Miracle.
And with that melatonin discussion, I symbolically put this thing to bed -- for another long sleep!
-Michael
Representative 2-week CRON-O-Meter:
References
1: Strong R, Miller RA, Antebi A, Astle CM, Bogue M, Denzel MS, Fernandez E, Flurkey K, Hamilton KL, Lamming DW, Javors MA, de Magalhães JP, Martinez PA, McCord JM, Miller BF, Müller M, Nelson JF, Ndukum J, Rainger GE, Richardson A, Sabatini DM, Salmon AB, Simpkins JW, Steegenga WT, Nadon NL, Harrison DE. Longer lifespan in male mice treated with a weakly estrogenic agonist, an antioxidant, an α-glucosidase inhibitor or a Nrf2-inducer. Aging Cell. 2016 Oct;15(5):872-84. doi: 10.1111/acel.12496. Epub 2016 Jun 16. PubMed PMID: 27312235; PubMed Central PMCID: PMC5013015.
2: Harrison DE, Strong R, Allison DB, Ames BN, Astle CM, Atamna H, Fernandez E, Flurkey K, Javors MA, Nadon NL, Nelson JF, Pletcher S, Simpkins JW, Smith D, Wilkinson JE, Miller RA. Acarbose, 17-α-estradiol, and nordihydroguaiaretic acid extend mouse lifespan preferentially in males. Aging Cell. 2014 Apr;13(2):273-82. doi: 10.1111/acel.12170. Epub 2013 Nov 19. PubMed PMID: 24245565; PubMed Central PMCID: PMC3954939.
3: Pearson KJ, Baur JA, Lewis KN, Peshkin L, Price NL, Labinskyy N, Swindell WR, Kamara D, Minor RK, Perez E, Jamieson HA, Zhang Y, Dunn SR, Sharma K, Pleshko N, Woollett LA, Csiszar A, Ikeno Y, Le Couteur D, Elliott PJ, Becker KG, Navas P, Ingram DK, Wolf NS, Ungvari Z, Sinclair DA, de Cabo R (August 2008). "Resveratrol delays age-related deterioration and mimics transcriptional aspects of dietary restriction without extending life span". Cell Metab. 8 (2): 157–68. PMC 2538685 Freely accessible. PMID 18599363. doi:10.1016/j.cmet.2008.06.011.
4: Miller RA, Harrison DE, Astle CM, Baur JA, Boyd AR, de Cabo R, Fernandez E, Flurkey K, Javors MA, Nelson JF, Orihuela CJ, Pletcher S, Sharp ZD, Sinclair D, Starnes JW, Wilkinson JE, Nadon NL, Strong R (February 2011). "Rapamycin, but not resveratrol or simvastatin, extends life span of genetically heterogeneous mice". J. Gerontol. A Biol. Sci. Med. Sci. 66 (2): 191–201. PMC 3021372 Freely accessible. PMID 20974732. doi:10.1093/gerona/glq178.
5: Strong, Randy; Richard A. Miller; Clinton M. Astle; Joseph A. Baur; Rafael de Cabo; Elizabeth Fernandez; Wen Guo; Martin Javors; James L. Kirkland; James F. Nelson; David A. Sinclair; Bruce Teter; David Williams; Nurulain Zaveri; Nancy L. Nadon; David E. Harrison (January 2013). "Evaluation of Resveratrol, Green Tea Extract, Curcumin, Oxaloacetic Acid, and Medium-Chain Triglyceride Oil on Life Span of Genetically Heterogeneous Mice". J Gerontol A Biol Sci Med Sci. 68 (1): 6–16. PMC 3598361 Freely accessible. PMID 22451473. doi:10.1093/gerona/gls070.
5a: da Luz, PL; Tanaka L; Brum PC; Dourado PM; Favarato D; Krieger JE; Laurindo FR (September 2012). "Red wine and equivalent oral pharmacological doses of Resveratrol delay vascular aging but do not extend life span in rats". Atherosclerosis. 224 (1): 136–42. PMID 22818625. doi:10.1016/j.atherosclerosis.2012.06.007.
6: Sensi M, De Rossi MG, Celi FS, Cristina A, Rosati C, Perrett D, Andreani D, Di Mario U. D-lysine reduces the non-enzymatic glycation of proteins in experimental diabetes mellitus in rats. Diabetologia. 1993 Sep;36(9):797-801. PMID: 8405749 [PubMed - indexed for MEDLINE]
7. Jyothirmayi GN, Modak R, Reddi AS. L-lysine reduces nonenzymatic glycation of glomerular basement membrane collagen and albuminuria in diabetic rats. Nephron. 2001 Feb;87(2):148-54. PMID: 11244310 [PubMed - indexed for MEDLINE]
8: Sulochana KN, Punitham R, Ramakrishnan S. Beneficial effect of lysine and amino acids on cataractogenesis in experimental diabetes through possible antiglycation of lens proteins. Exp Eye Res. 1998 Nov;67(5):597-601. PubMed PMID: 9878222.
9: Zhu W, Wang Z, Tang WHW, Hazen SL. Gut Microbe-Generated Trimethylamine N-Oxide From Dietary Choline Is Prothrombotic in Subjects. Circulation. 2017 Apr 25;135(17):1671-1673. doi: 10.1161/CIRCULATIONAHA.116.025338. PubMed PMID: 28438808; PubMed Central PMCID: PMC5460631.
10: Cho CE, Taesuwan S, Malysheva OV, Bender E, Tulchinsky NF, Yan J, Sutter JL, Caudill MA. Trimethylamine-N-oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: A randomized controlled trial. Mol Nutr Food Res. 2017 Jan;61(1). doi: 10.1002/mnfr.201600324. Epub 2016 Aug 3. PubMed PMID: 27377678.
11: Romano KA, Vivas EI, Amador-Noguez D, Rey FE. Intestinal microbiota composition modulates choline bioavailability from diet and accumulation of the proatherogenic metabolite trimethylamine-N-oxide. MBio. 2015 Mar 17;6(2):e02481. doi: 10.1128/mBio.02481-14. PubMed PMID: 25784704; PubMed Central PMCID: PMC4453578.
12: Martin FP, Wang Y, Sprenger N, Yap IK, Lundstedt T, Lek P, Rezzi S, Ramadan Z, van Bladeren P, Fay LB, Kochhar S, Lindon JC, Holmes E, Nicholson JK. Probiotic modulation of symbiotic gut microbial-host metabolic interactions in a humanized microbiome mouse model. Mol Syst Biol. 2008;4:157. doi: 10.1038/msb4100190. Epub 2008 Jan 15. PubMed PMID: 18197175; PubMed Central PMCID: PMC2238715.
13. Contreras I, Reiser KM, Martinez N, Giansante E, Lopez T, Suarez N, Postalian S, Molina M, Gonzalez F, Sanchez MR, Camejo M, Blanco MC. Effects of aspirin or basic amino acids on collagen cross-links and complications in NIDDM. Diabetes Care. 1997 May;20(5):832-5. PMID: 9135951
14: Wu ET, Liang JT, Wu MS, Chang KC. Pyridoxamine prevents age-related aortic stiffening and vascular resistance in association with reduced collagen glycation. Exp Gerontol. 2011 Jun;46(6):482-8. doi: 10.1016/j.exger.2011.02.001. Epub 2011 Feb 18. PubMed PMID: 21316441. [In the full text, they reveal no effects on nondiabetic animals; this is not the only case].
15: Williams ME, Bolton WK, Khalifah RG, Degenhardt TP, Schotzinger RJ, McGill JB. Effects of pyridoxamine in combined phase 2 studies of patients with type 1 and type 2 diabetes and overt nephropathy. Am J Nephrol. 2007;27(6):605-14. Epub 2007 Sep 6. PubMed PMID: 17823506.
16: Mills KF, Yoshida S, Stein LR, Grozio A, Kubota S, Sasaki Y, Redpath P, Migaud ME, Apte RS, Uchida K, Yoshino J, Imai SI. Long-Term Administration of Nicotinamide Mononucleotide Mitigates Age-Associated Physiological Decline in Mice. Cell Metab. 2016 Dec 13;24(6):795-806. doi: 10.1016/j.cmet.2016.09.013. Epub 2016 Oct 27. PubMed PMID: 28068222.
16a: Zhang H, Ryu D, Wu Y, Gariani K, Wang X, Luan P, D'Amico D, Ropelle ER, Lutolf MP, Aebersold R, Schoonjans K, Menzies KJ, Auwerx J. NAD⁺ repletion improves mitochondrial and stem cell function and enhances life span in mice. Science. 2016 Jun 17;352(6292):1436-43. doi: 10.1126/science.aaf2693. Epub 2016 Apr 28. PubMed PMID: 27127236.
16b: Zhu XH, Lu M, Lee BY, Ugurbil K, Chen W. In vivo NAD assay reveals the intracellular NAD contents and redox state in healthy human brain and their age dependences. Proc Natl Acad Sci U S A. 2015 Mar 3;112(9):2876-81. doi: 10.1073/pnas.1417921112. Epub 2015 Feb 17. PubMed PMID: 25730862; PubMed Central PMCID: PMC4352772.
16c: Massudi H, Grant R, Braidy N, Guest J, Farnsworth B, Guillemin GJ. Age-associated changes in oxidative stress and NAD+ metabolism in human tissue. PLoS One. 2012;7(7):e42357. doi: 10.1371/journal.pone.0042357. Epub 2012 Jul 27. PubMed PMID: 22848760; PubMed Central PMCID: PMC3407129.
17. Zittermann A, Iodice S, Pilz S, Grant WB, Bagnardi V, Gandini S. Vitamin D deficiency and mortality risk in the general population: a meta-analysis of prospective cohort studies. Am J Clin Nutr. 2011 Dec 14. [Epub ahead of print] PubMed PMID: 22170374.
18: Rae C, Digney AL, McEwan SR, Bates TC. Oral creatine monohydrate supplementation improves brain performance: a double-blind, placebo-controlled, cross-over trial. Proc Biol Sci. 2003 Oct 22;270(1529):2147-50. PubMed PMID: 14561278; PubMed Central PMCID: PMC1691485.
19. Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysisof 34 prospective studies. Arch Intern Med. 2006 Dec 11-25;166(22):2437-45. PubMed PMID: 17159008.
20. Streppel MT, Ocké MC, Boshuizen HC, Kok FJ, Kromhout D. Long-term wine consumption is related tocardiovascular mortality and life expectancy independently of moderate alcohol intake: the Zutphen Study. J Epidemiol Community Health. 2009 Jul;63(7):534-40. PubMed PMID: 19406740.
21: Brzezinski A, Vangel MG, Wurtman RJ, Norrie G, Zhdanova I, Ben-Shushan A, Ford I. Effects of exogenous melatonin on sleep: a meta-analysis. Sleep Med Rev. 2005 Feb;9(1):41-50. PubMed PMID: 15649737.
22: Zhdanova IV, Wurtman RJ, Morabito C, Piotrovska VR, Lynch HJ. Effects of low oral doses of melatonin, given 2-4 hours before habitual bedtime, on sleep in normal young humans. Sleep. 1996 Jun;19(5):423-31. PubMed PMID: 8843534.
23: Zhdanova IV, Wurtman RJ, Lynch HJ, Ives JR, Dollins AB, Morabito C, Matheson JK, Schomer DL. Sleep-inducing effects of low doses of melatonin ingested in the evening. Clin Pharmacol Ther. 1995 May;57(5):552-8. PubMed PMID: 7768078.
24. Schrauzer GN. Lithium: occurrence, dietary intakes, nutritional essentiality. J Am Coll Nutr. 2002 Feb ;21 (1):14-21. PMID 11838882
25. Ohgami H, Terao T, Shiotsuki I, Ishii N, Iwata N. Lithium levels in drinking water and risk of suicide. Br J Psychiatry. 2009 May ;194 (5):464-5; discussion 446. PMID 19407280
26: Trammell SA, Schmidt MS, Weidemann BJ, Redpath P, Jaksch F, Dellinger RW, Li Z, Abel ED, Migaud ME, Brenner C. Nicotinamide riboside is uniquely and orally bioavailable in mice and humans. Nat Commun. 2016 Oct 10;7:12948. doi: 10.1038/ncomms12948. PubMed PMID: 27721479; PubMed Central PMCID: PMC5062546.
27: Liu M, Li L, Chu J, Zhu B, Zhang Q, Yin X, Jiang W, Dai G, Ju W, Wang Z, Yang Q, Fang Z. Serum N(1)-Methylnicotinamide Is Associated With Obesity and Diabetes in Chinese. J Clin Endocrinol Metab. 2015 Aug;100(8):3112-7. doi: 10.1210/jc.2015-1732. Epub 2015 Jun 12. PubMed PMID: 26066674; PubMed Central PMCID: PMC4525009.
27a: Zhou SS, Li D, Zhou Y. Letter to the Editor: High Serum N(1)-Methylnicotinamide in Obesity and Diabetes: A Consequence of Excess Nicotinamide? J Clin Endocrinol Metab. 2015 Sep;100(9):L78-9. doi: 10.1210/jc.2015-2711. PubMed PMID: 26339743.
27b: Kannt A, Pfenninger A, Teichert L, Tönjes A, Dietrich A, Schön MR, Klöting N, Blüher M. Association of nicotinamide-N-methyltransferase mRNA expression in human adipose tissue and the plasma concentration of its product, 1-methylnicotinamide, with insulin resistance. Diabetologia. 2015 Apr;58(4):799-808. doi: 10.1007/s00125-014-3490-7. Epub 2015 Jan 18. PubMed PMID: 25596852; PubMed Central PMCID: PMC4351435.
27c: Zhou SS, Li D, Sun WP, Guo M, Lun YZ, Zhou YM, Xiao FC, Jing LX, Sun SX, Zhang LB, Luo N, Bian FN, Zou W, Dong LB, Zhao ZG, Li SF, Gong XJ, Yu ZG, Sun CB, Zheng CL, Jiang DJ, Li ZN. Nicotinamide overload may play a role in the development of type 2 diabetes. World J Gastroenterol. 2009 Dec 7;15(45):5674-84. PubMed PMID: 19960564; PubMed Central PMCID: PMC2789220.
27d: Salek RM, Maguire ML, Bentley E, Rubtsov DV, Hough T, Cheeseman M, Nunez D, Sweatman BC, Haselden JN, Cox RD, Connor SC, Griffin JL. A metabolomic comparison of urinary changes in type 2 diabetes in mouse, rat, and human. Physiol Genomics. 2007 Apr 24;29(2):99-108. Epub 2006 Dec 26. PubMed PMID: 17190852.
27e: Friedrich N, Skaaby T, Pietzner M, Budde K, Thuesen BH, Nauck M, Linneberg A. Identification of urine metabolites associated with 5-year changes in biomarkers of glucose homoeostasis. Diabetes Metab. 2017 Jun 29. pii: S1262-3636(17)30105-2. doi: 10.1016/j.diabet.2017.05.007. [Epub ahead of print] PubMed PMID: 28669514.
27f: Ellero-Simatos S, Szymańska E, Rullmann T, Dokter WH, Ramaker R, Berger R, van Iersel TM, Smilde AK, Hankemeier T, Alkema W. Assessing the metabolic effects of prednisolone in healthy volunteers using urine metabolic profiling. Genome Med. 2012 Nov 30;4(11):94. doi: 10.1186/gm395. eCollection 2012. PubMed PMID: 23199229; PubMed Central PMCID: PMC4064315.
27g: Goldie C, Taylor AJ, Nguyen P, McCoy C, Zhao XQ, Preiss D. Niacin therapy and the risk of new-onset diabetes: a meta-analysis of randomised controlled trials. Heart. 2016 Feb;102(3):198-203. doi: 10.1136/heartjnl-2015-308055. Epub 2015 Sep 14. PubMed PMID: 26370223; PubMed Central PMCID: PMC4752613.
28: Kraus D, Yang Q, Kong D, Banks AS, Zhang L, Rodgers JT, Pirinen E, Pulinilkunnil TC, Gong F, Wang YC, Cen Y, Sauve AA, Asara JM, Peroni OD, Monia BP, Bhanot S, Alhonen L, Puigserver P, Kahn BB. Nicotinamide N-methyltransferase knockdown protects against diet-induced obesity. Nature. 2014 Apr 10;508(7495):258-62. doi: 10.1038/nature13198. PubMed PMID: 24717514; PubMed Central PMCID: PMC4107212.
29: Williams A, Ramsden D. Nicotinamide: a double edged sword. Parkinsonism Relat Disord. 2005 Nov;11(7):413-20. Epub 2005 Sep 23. Review. PubMed PMID: 16183323.
30: Fukushima T. Niacin metabolism and Parkinson's disease. Environ Health Prev Med. 2005 Jan;10(1):3-8. doi: 10.1265/ehpm.10.3. PubMed PMID: 21432157; PubMed Central PMCID: PMC2723628.
31: Liu M, Chu J, Gu Y, Shi H, Zhang R, Wang L, Chen J, Shen L, Yu P, Chen X, Ju W, Wang Z. Serum N1-Methylnicotinamide is Associated With Coronary Artery Disease in Chinese Patients. J Am Heart Assoc. 2017 Feb 7;6(2). pii: e004328. doi: 10.1161/JAHA.116.004328. PubMed PMID: 28174167; PubMed Central PMCID: PMC5523749.
32. Zarse K, Terao T, Tian J, Iwata N, Ishii N, Ristow M. Low-dose lithium uptake promotes longevity in humans and metazoans. Eur J Nutr. 2011 Feb 8. [Epub ahead of print] PubMed PMID: 21301855.
32: Yamori Y, Liu L, Mori M, Sagara M, Murakami S, Nara Y, Mizushima S. Taurine as the nutritional factor for the longevity of the Japanese revealed by a world-wide epidemiological survey. Adv Exp Med Biol. 2009;643:13-25. PubMed PMID: 19239132.
33: Laura Della Corte (Editor), Ryan J. Huxtable (Editor), Giampietro Sgaragli (Editor), Keith F. Tipton (Editor). Taurine 4: Taurine and Excitable Tissues: Taurine and Excitable Tissues No. 4 (Advances in Experimental Medicine and Biology Volume 483). ISBN (9780306464478) . See here (Fig. 3) and here (Fig. 1).
34: Chini CC, Tarragó MG, Chini EN. NAD and the aging process: Role in life, death and everything in between. Mol Cell Endocrinol. 2016 Nov 5. pii: S0303-7207(16)30462-2. doi: 10.1016/j.mce.2016.11.003. [Epub ahead of print] PubMed PMID: 27825999; PubMed Central PMCID: PMC5419884.
35: Villareal DT, Kotyk JJ, Armamento-Villareal RC, Kenguva V, Seaman P, Shahar A, Wald MJ, Kleerekoper M, Fontana L. Reduced bone mineral density is not associated with significantly reduced bone quality in men and women practicing long-term calorie restriction with adequate nutrition. Aging Cell. 2011 Feb;10(1):96-102. doi: 10.1111/j.1474-9726.2010.00643.x. Epub 2010 Nov 15. PubMed PMID: 20969721.
36. Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, Britt EB, Fu X, Wu Y, Li L, Smith JD, Didonato JA, Chen J, Li H, Wu GD, Lewis JD, Warrier M, Brown JM, Krauss RM, Tang WH, Bushman FD, Lusis AJ, Hazen SL. Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013 May;19(5):576-85. doi: 10.1038/nm.3145. Epub 2013 Apr 7. PubMed PMID: 23563705; PubMed Central PMCID: PMC3650111.
37. Pepino MY, Tiemann CD, Patterson BW, Wice BM, Klein S. Sucralose Affects Glycemic and Hormonal Responses to an Oral Glucose Load. Diabetes Care. 2013 Apr 30. [Epub ahead of print] PubMed PMID: 23633524.
38. Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Wine, beer or spirit drinking in relation to fatal and non-fatal cardiovascular events: a meta-analysis. Eur J Epidemiol. 2011 Nov;26(11):833-50. doi: 10.1007/s10654-011-9631-0. Epub 2011 Nov 11. PubMed PMID: 22076059.
39 Sabrina Moret; Annalisa Prevarin; Franco Tubaro. Levels of creatine, organic contaminants and heavy metals in creatine dietary supplements. Food Chemistry 2011 Jun;126(3): 1232-1238 DOI: 10.1016/j.foodchem.2010.12.028
40: Barger JL, Vann JM, Cray NL, Pugh TD, Mastaloudis A, Hester SN, Wood SM, Newton MA, Weindruch R, Prolla TA. Identification of tissue-specific transcriptional markers of caloric restriction in the mouse and their use to evaluate caloric restriction mimetics. Aging Cell. 2017 Aug;16(4):750-760. doi: 10.1111/acel.12608. Epub 2017 May 26. PubMed PMID: 28556428; PubMed Central PMCID: PMC5506434.
41: Spindler SR, Mote PL, Flegal JM. Lifespan effects of simple and complex nutraceutical combinations fed isocalorically to mice. Age (Dordr). 2014 Apr;36(2):705-18. doi: 10.1007/s11357-013-9609-9. Epub 2013 Dec 28. PubMed PMID: 24370781; PubMed Central PMCID: PMC4039264.
42: Barger JL, Anderson RM, Newton MA, da Silva C, Vann JA, Pugh TD, Someya S, Prolla TA, Weindruch R. A conserved transcriptional signature of delayed aging and reduced disease vulnerability is partially mediated by SIRT3. PLoS One. 2015 Apr 1;10(4):e0120738. doi: 10.1371/journal.pone.0120738. eCollection 2015. PubMed PMID: 25830335; PubMed Central PMCID: PMC4382298.
43: Wegman MP, Guo MH, Bennion DM, Shankar MN, Chrzanowski SM, Goldberg LA, Xu J, Williams TA, Lu X, Hsu SI, Anton SD, Leeuwenburgh C, Brantly ML. Practicality of intermittent fasting in humans and its effect on oxidative stress and genes related to aging and metabolism. Rejuvenation Res. 2015 Apr;18(2):162-72. doi: 10.1089/rej.2014.1624. PubMed PMID: 25546413; PubMed Central PMCID: PMC4403246.
44: Baguet A, Everaert I, De Naeyer H, Reyngoudt H, Stegen S, Beeckman S, Achten E, Vanhee L, Volkaert A, Petrovic M, Taes Y, Derave W. Effects of sprint training combined with vegetarian or mixed diet on muscle carnosine content and buffering capacity. Eur J Appl Physiol. 2011 Oct;111(10):2571-80. doi: 10.1007/s00421-011-1877-4. Epub 2011 Mar 4. PubMed PMID: 21373871.
45: Everaert I, Mooyaart A, Baguet A, Zutinic A, Baelde H, Achten E, Taes Y, De Heer E, Derave W. Vegetarianism, female gender and increasing age, but not CNDP1 genotype, are associated with reduced muscle carnosine levels in humans. Amino Acids. 2011 Apr;40(4):1221-9. doi: 10.1007/s00726-010-0749-2. Epub 2010 Sep 24. PubMed PMID: 20865290.
46: Stegen S, Blancquaert L, Everaert I, Bex T, Taes Y, Calders P, Achten E, Derave W. Meal and beta-alanine coingestion enhances muscle carnosine loading. Med Sci Sports Exerc. 2013 Aug;45(8):1478-85. doi: 10.1249/MSS.0b013e31828ab073. PubMed PMID: 23439427.
47: Skagen K, Trøseid M, Ueland T, Holm S, Abbas A, Gregersen I, Kummen M, Bjerkeli V, Reier-Nilsen F, Russell D, Svardal A, Karlsen TH, Aukrust P, Berge RK, Hov JE, Halvorsen B, Skjelland M. The Carnitine-butyrobetaine-trimethylamine-N-oxide pathway and its association with cardiovascular mortality in patients with carotid atherosclerosis. Atherosclerosis. 2016 Apr;247:64-9. doi: 10.1016/j.atherosclerosis.2016.01.033. Epub 2016 Feb 5. PubMed PMID: 26868510.
48: Koeth RA, Levison BS, Culley MK, Buffa JA, Wang Z, Gregory JC, Org E, Wu Y, Li L, Smith JD, Tang WH, DiDonato JA, Lusis AJ, Hazen SL. γ-Butyrobetaine is a proatherogenic intermediate in gut microbial metabolism of L-carnitine to TMAO. Cell Metab. 2014 Nov 4;20(5):799-812. doi: 10.1016/j.cmet.2014.10.006. Epub 2014 Nov 4. PubMed PMID: 25440057; PubMed Central PMCID: PMC4255476.
49: Bain MA, Milne RW, Evans AM. Disposition and metabolite kinetics of oral L-carnitine in humans. J Clin Pharmacol. 2006 Oct;46(10):1163-70. PubMed PMID: 16988205.
50: Paroni R, Cighetti G, Del Puppo M, Kienle MG. Evidence for a different metabolic behaviour of cytidine diphosphate choline after oral and intravenous administration to rats. Pharmacol Res Commun. 1985 Sep;17(9):805-29. PubMed PMID: 4059318.
51: Weimer S, Priebs J, Kuhlow D, Groth M, Priebe S, Mansfeld J, Merry TL, Dubuis S, Laube B, Pfeiffer AF, Schulz TJ, Guthke R, Platzer M, Zamboni N, Zarse K, Ristow M. D-Glucosamine supplementation extends life span of nematodes and of ageing mice. Nat Commun. 2014 Apr 8;5:3563. doi: 10.1038/ncomms4563. PubMed PMID: 24714520; PubMed Central PMCID: PMC3988823.
52: Moskalev A, Chernyagina E, Tsvetkov V, Fedintsev A, Shaposhnikov M, Krut'ko V, Zhavoronkov A, Kennedy BK. Developing criteria for evaluation of geroprotectors as a key stage toward translation to the clinic. Aging Cell. 2016 Jun;15(3):407-15. doi: 10.1111/acel.12463. Epub 2016 Mar 11. Review. PubMed PMID: 26970234; PubMed Central PMCID: PMC4854916.
53: Kantor ED, Zhang X, Wu K, Signorello LB, Chan AT, Fuchs CS, Giovannucci EL. Use of glucosamine and chondroitin supplements in relation to risk of colorectal cancer: Results from the Nurses' Health Study and Health Professionals follow-up study. Int J Cancer. 2016 Nov 1;139(9):1949-57. doi: 10.1002/ijc.30250. Epub 2016 Jul 18. PubMed PMID: 27357024; PubMed Central PMCID: PMC4990485.
54: Knapen MH, Drummen NE, Smit E, Vermeer C, Theuwissen E. Three-year low-dose menaquinone-7 supplementation helps decrease bone loss in healthy postmenopausal women. Osteoporos Int. 2013 Sep;24(9):2499-507. doi: 10.1007/s00198-013-2325-6. Epub 2013 Mar 23. PubMed PMID: 23525894.
55: Rønn SH, Harsløf T, Pedersen SB, Langdahl BL. Vitamin K2 (menaquinone-7) prevents age-related deterioration of trabecular bone microarchitecture at the tibia in postmenopausal women. Eur J Endocrinol. 2016 Dec;175(6):541-549. Epub 2016 Sep 13. PubMed PMID: 27625301.
56: Hine C, Kim HJ, Zhu Y, Harputlugil E, Longchamp A, Matos MS, Ramadoss P, Bauerle K, Brace L, Asara JM, Ozaki CK, Cheng SY, Singha S, Ahn KH, Kimmelman A, Fisher FM, Pissios P, Withers DJ, Selman C, Wang R, Yen K, Longo VD, Cohen P, Bartke A, Kopchick JJ, Miller R, Hollenberg AN, Mitchell JR. Hypothalamic-Pituitary Axis Regulates Hydrogen Sulfide Production. Cell Metab. 2017 Jun 6;25(6):1320-1333.e5. doi: 10.1016/j.cmet.2017.05.003. PubMed PMID: 28591635.
57: Nakano S, Ishii I, Shinmura K, Tamaki K, Hishiki T, Akahoshi N, Ida T, Nakanishi T, Kamata S, Kumagai Y, Akaike T, Fukuda K, Sano M, Suematsu M. Hyperhomocysteinemia abrogates fasting-induced cardioprotection against ischemia/reperfusion by limiting bioavailability of hydrogen sulfide anions. J Mol Med (Berl). 2015 Aug;93(8):879-89. doi: 10.1007/s00109-015-1271-5. Epub 2015 Mar 6. PubMed PMID: 25740079.
58: Hine C, Harputlugil E, Zhang Y, Ruckenstuhl C, Lee BC, Brace L, Longchamp A, Treviño-Villarreal JH, Mejia P, Ozaki CK, Wang R, Gladyshev VN, Madeo F, Mair WB, Mitchell JR. Endogenous hydrogen sulfide production is essential for dietary restriction benefits. Cell. 2015 Jan 15;160(1-2):132-44. doi: 10.1016/j.cell.2014.11.048. Epub 2014 Dec 23. PubMed PMID: 25542313; PubMed Central PMCID: PMC4297538.
59: Hine C, Mitchell JR. Calorie restriction and methionine restriction in control of endogenous hydrogen sulfide production by the transsulfuration pathway. Exp Gerontol. 2015 Aug;68:26-32. doi: 10.1016/j.exger.2014.12.010. Epub 2014 Dec 16. Review. PubMed PMID: 25523462; PubMed Central PMCID: PMC4464900.
60: Sun Q, Wang B, Li Y, Sun F, Li P, Xia W, Zhou X, Li Q, Wang X, Chen J, Zeng X, Zhao Z, He H, Liu D, Zhu Z. Taurine Supplementation Lowers Blood Pressure and Improves Vascular Function in Prehypertension: Randomized, Double-Blind, Placebo-Controlled Study. Hypertension. 2016 Mar;67(3):541-9. doi: 10.1161/HYPERTENSIONAHA.115.06624. Epub 2016 Jan 18. PubMed PMID: 26781281.
59: Katsyuba E, Auwerx J. Modulating NAD(+) metabolism, from bench to bedside. EMBO J. 2017 Aug 7. pii: e201797135. doi: 10.15252/embj.201797135. [Epub ahead of print] Review. PubMed PMID: 28784597.
60: Esfandiari H, Pakravan M, Zakeri Z, Ziaie S, Pakravan P, Ownagh V. Effect of glucosamine on intraocular pressure: a randomized clinical trial. Eye (Lond). 2017 Mar;31(3):389-394. doi: 10.1038/eye.2016.221. Epub 2016 Oct 21. PubMed PMID: 27768119; PubMed Central PMCID: PMC5350357.
61: Murphy RK, Ketzler L, Rice RD, Johnson SM, Doss MS, Jaccoma EH. Oral glucosamine supplements as a possible ocular hypertensive agent. JAMA Ophthalmol. 2013 Jul;131(7):955-7. doi: 10.1001/jamaophthalmol.2013.227. PubMed PMID: 23702812.