Great paper below.
https://www.ncbi.nlm...les/PMC6007750/
Mitochondrial Agents for Bipolar Disorder
N-Acetyl Cysteine
N-acetyl cysteine (NAC) is increasingly being used as an adjunctive therapy in psychiatry (Berk et al., 2013). Its use across psychiatric disorders is due to the number of mechanisms of action relevant to mental illness. In addition to providing rate-limiting cysteine for glutathione production, NAC has also been shown to be an antiinflammatory, enhance neurogenesis, decrease apoptosis, modulate glutamate pathways, and, importantly, alter mitochondrial activity (Samuni et al., 2013). In both mouse (R6/1) and rat (3-nitropropionic acid) models of Huntington’s Disease, NAC has been shown to restore mitochondrial respiration (Wright et al., 2015) and complex activity (Sandhir et al., 2012). Restoration of mitochondrial respiration has also been shown in rat models of traumatic brain injury as well as improvements in mitochondrial complex activity and mitochondrial glutathione (Patel et al., 2014).
There is promising clinical evidence in support of adjunctive NAC in diverse psychiatric disorders (Deepmala et al., 2015). A systematic review and meta-analysis has shown that overall, adjunctive NAC treatment seems beneficial for both unipolar and bipolar depression (Fernandes et al., 2016).
To date, there have been 2 multi-site trials of NAC specifically exploring its use as an adjunctive treatment for BD. Several substudies have also been reported from these data. The initial study was conducted in participants with BD (n=75) that were experiencing any symptoms (or euthymic). At 6 months post-baseline, participants that received 2000 mg/d NAC (in addition to standard treatment) reported improved measures of BD symptoms, functioning, and quality of life. This improvement persisted up to 4 weeks following NAC treatment cessation. Adverse effects did not significantly differ between the NAC and placebo groups (Berk et al., 2008).
Posthoc exploratory analyses were performed on a variety of data from this trial to assist in identifying who might benefit most from adjunctive NAC treatment in BD. This series of studies included the investigation of mania (or hypomania), bipolar II, major depressive episodes, cognition and comorbid systemic illness (Magalhães et al. 2011a, 2011b, 2013; Dean et al., 2012). When exploring major depressive episodes within the context of a BD sample, there were improvements following adjunctive NAC compared with placebo (Magalhães et al., 2011b). The investigation of those experiencing mania indicated within-group improvements in the NAC group (Magalhães et al., 2013). Similarly, when exploring a subgroup of participants (n=14) with bipolar II (divided in 2 groups of 7 patients each randomized to placebo or NAC), NAC was found to improve symptoms in 6/7 participants, compared with 2/7 in the placebo group (Magalhães et al., 2011a). NAC was also shown to improve functional outcomes for people experiencing cardiovascular or endocrine comorbidities when compared to those who did not (Magalhães et al., 2012). Finally, a paper on posthoc analyses has reported no change in cognition in a small subset of participants following NAC (Dean et al., 2012).
The next study included a maintenance design with an initial open-label phase. Participants were given 2000 mg/d of NAC (n=149) for a total of 8 weeks and were then randomized to continuation of adjunctive NAC treatment or a placebo. The open-label phase showed significant improvements in participants experiencing bipolar depression (Berk et al., 2011). However, in the maintenance (randomized) phase, participants in both arms generally stayed well, which resulted in no significant treatment effects (Berk et al., 2012).
We further searched ANZCTR and Clinicaltrials.gov to ascertain if there are upcoming studies in this area. A protocol has been published describing a study of NAC and a combination of other agents that enhance mitochondrial function, compared with placebo, over 16 weeks of treatment (Dean et al., 2015).
Overall, NAC is a potentially useful adjunctive therapy for BD and, in particular, bipolar depression during the acute phase. NAC has been shown to enhance mitochondrial function in preclinical models. However, no clinical studies that have investigated NAC for BD have evaluated outcomes related to mitochondrial function. Further research is required to explore the interactions of NAC clinical efficacy and changes in relevant pathways, including pathways relevant to mitochondrial function.
Coenzyme Q10 (CoQ10), also known as ubiquinone, is a powerful lipid-soluble antioxidant that reduces the flow of electrons on the ROS-producing regions of Complex I, II, and III of the mitochondria (Lenaz et al., 2002; Nierenberg et al., 2013). CoQ10 reduces ROS by neutralizing the free radical alpha-tocopheroxyl to alpha-tocopherol (vitamin E) and plays a role in the biosynthesis of adenosine triphosphate (ATP) (Morris et al., 2013; Nierenberg et al., 2013). The genes associated with these complexes and the transportation of electrons across them are expressed differently in BD compared with healthy controls (Sun et al., 2006b). Supplementary CoQ10 has poor oral bioavailability; however, it does cross the blood-brain barrier (Matthews et al., 1998).
Morris et al. (2013) discussed the reduction in CoQ10 levels in psychiatric and mitochondrial disorders such as depression, chronic fatigue syndrome, fibromyalgia, and Parkinson’s disease and postulated that CoQ10 supplementation could be a treatment for these disorders. However, a meta-analysis of CoQ10 supplementation compared with placebo showed no significant benefits for participants with Parkinson’s disease (Negida et al., 2016).
There have been several studies proposing the use of CoQ10 supplementation as a mitochondrial enhancing agent in general and for BD in particular (Morris et al., 2013; Nierenberg et al., 2013). Despite this, there have been only 2 studies directly looking at CoQ10 supplementation and BD. One study explored CoQ10 in combination with other mitochondrial agents (such as NAC and b-group vitamins) as an adjunctive treatment for bipolar depression (Dean et al., 2015). This study has been completed but results are still pending.
Forester et al. (2012) investigated an 8-week intervention of CoQ10 in a sample of 10 outpatients aged 55 years and older with a DSM-IV diagnosis of bipolar depression in an 8-week study. Participants were administered CoQ10 and compared with 8 healthy controls who did not receive CoQ10 supplementation. The maximum dose of CoQ10 was 1200 mg/d, starting at 400 mg/d and titrated up by 400 mg/d every 2 weeks. Participants on CoQ10 showed modest but significant improvements in their depression symptoms (measured on the Montgomery–Åsberg Depression Rating Scale MADRS) over the 8-week study. Furthermore, this study also investigated mitochondrial function via phosphorus magnetic resonance spectroscopy and reported no significant differences between groups for creatine kinase (a mitochondrial protein). This small study is limited by the sample size and lack of placebo control but highlights the potential of CoQ10 as an antidepressant and treatment for BD.
Alpha-lipoic acid (ALA), also known as thioctic acid, is a pleiotropic substance (Gomes and Negrato, 2014). ALA is a strong antioxidant (Suzuki et al., 1991; Moini et al., 2002). It increases levels of glutathione (Han et al., 1997; Yamada et al., 2011; Kleinkauf-Rocha et al., 2013), raises hepatocyte ascorbate levels (Lykkesfeldt et al., 1998; Michels et al., 2003), downregulates nuclear factor kappa-light-chain-enhancer of activated B cells (DeMarco et al., 2004), and is a metal chelator (Ou et al., 1995; Suh et al., 2005), an antiviral in glial cells (Scumpia et al., 2014), and a glucose uptake promoter (Estrada et al., 1996; Henriksen et al., 1997; Saengsirisuwan et al., 2004), increasing GLUT4 levels and insulin action (Hughes et al., 1993). Relevant to the current review, ALA also has a role as a mitochondrial agent. It can be endogenously synthesized in the mitochondria where it acts as a coenzyme for the formation of pyruvate dehydrogenase and α-ketoglutarate—both essential components of the Krebs cycle. Because pyruvate dehydrogenase converts pyruvate to acetyl CoA, ALA decreases lactate levels, thus inhibiting glycolysis (Gomes and Negrato, 2014). It also modulates the key regulator of mitochondrial biogenesis, peroxisome proliferator-activated receptor-gamma coactivator-1alpha (PPAR-GC-1α) (Liu, 2008). PPAR-GC-1α stimulation has been linked to neuroprotection and its suppression to mitochondrial dysfunction and neurodegeneration (Cui et al., 2006; St-Pierre et al., 2006). ALA also affects the mitochondrial pathway of apoptosis, prompting research in oncology as an agent with antimetastatic potential (Dörsam and Fahrer, 2016). This provides a rationale for its action in mood and cognitive disorders.
In a corticosterone-induced model of depression in mice, ALA showed antidepressant properties and reversed brain-derived neurotrophic factor reduction in the hippocampus and striatum (de Sousa et al., 2015). In a d-amphetamine-induced model of mania, ALA was able to both prevent and reverse symptoms with comparable efficiency to lithium (Macêdo et al., 2012).
Only one clinical trial has explored ALA as an adjunctive treatment for bipolar depression. The trial tested a combination of ALA (600–1800 mg/d) and acetyl-L-carnitine (ALC) (1000–3000 mg/d) or placebo for 12 weeks in 40 participants with bipolar depression. Previous treatment (stable for at least 4 weeks) was continued. The primary outcome was depression, measured on the MADRS. No significant changes were found between groups (Brennan et al., 2013). As the authors note, the shorter duration of the study (12 weeks) compared with a positive RCT of a mitochondrial agent (NAC) in BD (24 weeks) (Berk et al., 2008), the inclusion of bipolar I and II types, concomitant medication use, and possible low oral bioavailability of the agents are all potential confounders that should be addressed.
More research is required to determine the efficacy of ALA in BD. Moreover, there is one study (described earlier) in bipolar depression that is currently being completed that includes a combination of agents including ALA, ALC, and NAC (ACTRN12612000830897).
In addition to the role of ALC in mitochondrial β-oxidation and energy production (Hoppel, 2003), ALC has antioxidant properties (Gülçin, 2006; Mescka et al., 2011). Additionally, ALC has been proposed to mediate the transfer of acetyl groups for acetylcholine synthesis, modulate nerve growth factors and gene expression (Nałecz and Nałecz, 1996; Binienda, 2003; Nacz et al., 2004), and counter glutamate-induced excitotoxicity (Zanelli et al., 2005).
Data from animal models provide further evidence for ALC’s therapeutic potential due to its role as an antioxidant and in improving mitochondrial energy production (Rao et al., 1997; Aureli et al., 1998; Hagen et al., 2002b; Al-Majed et al., 2006), its neuroprotective action in trauma (Karalija et al., 2014) and ischemia (Rosenthal et al., 1992; Barhwal et al., 2007), its antidepressant effect in the forced swim test (FST) (Wang et al., 2015), and its ability to reverse memory loss in older rats (Liu et al., 2002).
Two patients with geriatric depression treated with ALC showed increases in PCr and β-nucleoside triphosphate (β-NTP) levels (Pettegrew et al., 2002). PCr serves as a reservoir for high-energy phosphates, and β-NTP is acknowledged as an index of brain levels of ATP. Thus, these results provide support for a link between the antidepressant action of ALC and improved energy production within the brain.
However, the only RCT in BD reported no effect when administered in combination with ALA (Brennan et al., 2013) (see above). Furthermore, the change in PCr and β-NTP, previously found in geriatric depression patients (Pettegrew et al., 2002), was not observed (Brennan et al., 2013). Two case reports of ALC-associated relapse in BD also suggest some caution with clinical use. The first case-reports detail a psychotic episode in a known BD type I patient, 5 days after starting treatment with nutritional supplements including vitamin C, vitamin E, and ALC (500 mg/d) (Evcimen et al., 2007). Manic symptoms associated with self-prescribed ALC treatment (2000 mg/d) in a man with BD type I resolved 3 days after cessation of ALC (Goodison et al., 2016).
S-Adenosylmethionine (SAMe) results from the combination of ATP and methionine and plays a crucial role as a methyl donor in reactions involving methyltrasnferases (Bottiglieri, 2002). SAMe is also a precursor molecule for glutathione production, which plays an essential role in reducing oxidative stress. In the brain, SAMe repairs and degrades proteins and activates thyroxine hydroxylase through methylation, which is critical in the synthesis and regulation of monoamines (i.e., dopamine, serotonin), which are known to be dysregulated in BD (Bottiglieri et al., 2000, 2002). Recently, an RCT of SAMe as an add-on to an approved mood stabilizer in 20 participants with BD (type I and II) was conducted. To enroll, subjects were required to have not responded previously to either 2 antidepressants (of different classes) or to 2 different mood stabilizers. No significant differences were observed in MADRS, Hamilton Rating Scale for Depression (HAM-D), or Young Mania Rating Scale (YMRS) between the SAMe and placebo groups. No switches to mania were reported (Murphy et al., 2014). Carney et al. (1989) reported 3 open label trials and 1 placebo-controlled trial after a drug-free period of at least 7 days. There were 14 unipolar depression and 11 BD participants. Nine of the 11 BD participants switched to hypomania, mania, or “elevated mood.” The other 2 participants did not respond to treatment (Carney et al., 1989). In an open-label trial of i.v. SAMe monotherapy for depression, 7 of 9 patients improved or had depression remission. There were 2 case reports of mood switch in BD patients, 1 of mania, and 1 of hypomania (Lipinski et al., 1984). Due to the potential for manic switching, SAMe for BD should be investigated with caution. In unipolar depression, a meta-analysis in 2002 showed that SAMe is superior to placebo improving HAM-D scores (Hardy et al., 2003). A recent systematic review collected clinical information from 115 clinical trials and 17 preclinical studies on the effect of SAMe on several neuropsychiatric conditions. Positive but limited evidence was found for the use of SAMe in major depressive disorder (MDD) as both a monotherapy and adjunctive therapy (Sharma et al., 2017). Recently, 2 studies have demonstrated benefits of SAMe as an augmentation antidepressant therapy. In a 6-week, double blind, placebo RCT with serotonin reuptake inhibitors or serotonin norepinephrine reuptake inhibitors nonresponders, participants undergoing SAMe augmentation had lower HAM-D score and higher remission rates (final HAM-D score <8) than placebo (Papakostas et al., 2010).
Creatine is the precursor of PCr. Long-term decrease of PCr decreases ATP production, attributable to mitochondrial dysfunction (Erecińska and Silver, 1989). Oral supplementation of creatine monohydrate increases creatine and brain concentrations of PCr (Dechent et al., 1999; Lyoo et al., 2003a). In BD, decreased PCr concentrations have been reported (Stork and Renshaw, 2005). Furthermore, creatine has been shown to have antioxidant properties in animal models of oxidative stress (Sullivan et al., 2000; Tarnopolsky and Beal, 2001; Lawler et al., 2002)
A 4-week open-label trial with 10 participants experiencing treatment-resistant depression (8 unipolar and 2 bipolar) showed improved depression scores with 3 to 5 g/d creatine monohydrate augmentation, provoking switch to elevated mood in both BD patients (Roitman et al., 2007). Two trials focusing on a combination of cytidine and creatine in bipolar depression are currently being conducted (NCT01543139; NCT02625779). A 6-week, double blind, placebo RCT to evaluate the efficacy of creatine monohydrate as an adjunctive therapy for BD type I depression (NCT01655030) is also currently recruiting.
Melatonin regulates several homeostatic processes such as circadian rhythm maintenance, growth hormone stimulation, and insulin secretion (Paredes et al., 2014; Simões et al., 2016; Zhang et al., 2016). Relevant to mitochondrial physiology, melatonin improves oxidative phosphorylation, increasing the activity of the I and IV dose-dependent complexes and membrane fluidity and closes the mitochondrial permeability transition pore (a protein complex spanning the inner and outer mitochondrial membranes), preventing ATP depletion and necrotic cell death (Acuña-Castroviejo et al., 2001, 2007; Martín et al., 2002; Leon et al., 2005). Moreover, melatonin and some of its metabolites play an important antiinflammatory and antioxidant role through scavenging oxygen and nitrogen-based ROS (López-Burillo et al., 2003; Korkmaz et al., 2009). Melatonin directly boosts mRNA expression of genes implicated in the production of glutathione peroxidase and superoxide dismutase, 2 antioxidant enzymes (Rodriguez et al., 2004; Acuña-Castroviejo et al., 2007; Anderson and Maes, 2014). Furthermore, peripheral melatonin, produced outside the brain, is decreased in BD compared with healthy controls, suggesting supplemental melatonin may be a relevant intervention in this population (Anderson and Maes, 2014).
In an 8-week, double blind, placebo control trial, 44 participants (24 participants with SZ and 20 with BD) treated with second-generation antipsychotics received low dosages of melatonin (5 mg/d) and placebo. The melatonin group showed lower diastolic blood pressure and less weight gain, these results being greater in the BD group (Romo-Nava et al., 2014). In an open-label trial, melatonin improved mania scale scores and sleeping patterns (Bersani and Garavini, 2000) but had no significant effects on mood or sleep in a double-blind, placebo-controlled trial using the same dose with 5 rapid-cycling DSM-III-R BD patients (Leibenluft et al., 1997).
McElroy et al. (2011) tested ramelteon (a highly selective melatonin MT1/MT2 receptor agonist) as an adjunctive treatment in 21 outpatients with bipolar I disorder with mild-to-moderate manic symptoms and sleep disturbance in an 8-week, double-blind, fixed-dose (8 mg/d) study. A global improvement in a global rating of depressive symptoms was reported; however, no significant differences in ratings of insomnia, mania, and global severity of illness were observed. Norris et al. (2013) conducted a double-blind, randomized, placebo-controlled trial of adjunctive ramelteon in euthymic bipolar patients with sleep disturbances and reported that participants receiving ramelteon were significantly less likely to relapse compared with placebo. Recently, a RCT comparing placebo with sublingual ramelteon in different dosages (0.1 mg, 0.4 mg, 0.8 mg, once daily) as adjunctive maintenance therapy in stable BD patients did not show significant differences between any dose of ramelteon and placebo (Mahableshwarkar et al., 2017). The study was terminated before the expected sample size due to meeting the futility criteria. All studies showed ramelteon was well tolerated and associated with no serious adverse events.
Agomelatine (an agonist of melatonin 1 and 2 receptors and antagonist of serotonin 2C receptors drug) has also been investigated as an adjunctive treatment for bipolar depression. In an open-label trial with 21 type I BD patients in a severe depressive episode (14 treated with lithium and 7 with valpromide), agomelatine was added at 25 mg/d for at least 6 weeks and, if participants opted-in, up to 1 year. At week 6, 81% of patients improved >50% in HAM-D score from baseline and almost 50% in the first study week. Three patients switched to mania or hypomania from the sixth week until the complete year follow-up (Calabrese et al., 2007). In a similar study, 28 type II BD patients in a severe depressive episode (11 treated with lithium and 17 with valproate) were treated with agomelatine at fixed dosages of 25 mg/d from at least 6 weeks to a possible 30-week extension. At 6 weeks, 64% of patients improved >50% in HAM-D score from baseline and 86% responded at 36 weeks. There were 4 drop-outs in total due to polarity change (1 manic and 3 hypomanic episodes) (Fornaro et al., 2013). Recently, 344 type I BD patients undergoing a current major depressive episode that were treated with lithium or valproic acid for at least 6 weeks were randomized to treatment with agomelatine or placebo (n=172 each group) in a double-blind study (Yatham et al., 2016). No significant differences between both groups in MADRS total score or response or remission rates from baseline to endpoint were found. The number of manic or hypomanic symptoms was comparable between both groups at each assessment time. As a number of sites had placebo response rates of 100%, when these were excluded in a posthoc analysis, a signal favoring agomelatine over placebo emerged. While the meta-analyses in unipolar depression confirm the antidepressant effects of agomelatine (Singh et al., 2012; Taylor et al., 2014), melatonin supplementation did not significantly improve treatment or prophylaxis of unipolar depression (Hansen et al., 2014).
The pyrimidine nucleosides such as uridine, triacetyluridine, and cytidine have effects on mitochondrial function, glutamatergic transmission, catecholamine synthesis, and cerebral phospholipid metabolism, which has been linked to the pathophysiology of BD (Yoon et al., 2009; Kondo et al., 2011). Uridine (1000 mg/d) was studied in a 6 weeks open-label trial of 7 teenagers with bipolar depression. Children’s Depression Rating Scale-Revised and the Clinical Global Impressions scale were used to measure the treatment results. Uridine was well tolerated and depressive symptoms decreased (Kondo et al., 2011).
In another 6-week study (n=20), 18 g/d day of triacetyluridine (TAU), a uridine prodrug, or placebo was given to patients with bipolar depression. BD patients who had a reduction in MADRS scores ≥50% showed a greater difference in pH changes (assessed by phosphorus magnetic resonance spectroscopic imaging (PMRSI)) compared with TAU nonresponders, suggesting that TAU treatment can have benefits in depressive symptoms and in mitochondrial function (Jensen et al., 2008). Cytidine, available from dietary sources and converted in uridine in the human body, was investigated in a 12-week, randomized, placebo trial with 35 patients with bipolar depression. Participants were randomly given valproate plus placebo or valproate plus cytidine. At 2, 4, and 12 weeks, the cerebral levels of glutamate/glutamine were measured using PMRSI. The results showed that cytidine supplementation resulted in earlier improvement in symptoms of depression and greater reduction in glutamate/glutamine levels. These data suggest that the observed therapeutic effect of cytidine may be mediated via a decrease in cerebral glutamate/glutamine levels (Yoon et al., 2009).
Choline is a constituent of the neurotransmitter acetylcholine, a major methyl-donor, and needed for structural integrity and intracellular signaling within cell membranes. In an open-label trial, Stoll et al. (1996) studied the effects of lithium augmentation with choline in 6 rapid-cycling BD outpatients. Five participants experienced a reduction in manic symptoms and 4 had a reduction in all mood symptoms during choline therapy. The impact on depression was variable. Lyoo et al. (2003b) studied 8 lithium-treated, rapid-cycling BD I and II patients randomized to receive either choline or placebo, and reported significantly decreased brain purine levels, a marker of energy metabolism.
Both deficient and excessive levels of vitamin A disrupt many human systems, including the central nervous system (CNS) (Chapman, 2012). Vitamin A is required for vision, gene transcription, immune system, and skin cell differentiation (Haybaeck et al., 2015). The role of vitamin A in gene expression and its role in redox activation suggest a possible role as a mitochondrial agent in the treatment of BD. Vitamin A also plays a very important role as a co-factor in redox activation, binding to protein kinase C (Hoyos et al., 2012; Hammerling, 2016). Retinoid receptors are concentrated in the striatum, hippocampus, frontal cortex, and hypothalamus, all key brain areas involved in depression (Bremner et al., 2012). Being involved in neuroplasticity in the hippocampus, vitamin A deficiency can also affect memory, appetite, and growth (Haybaeck et al., 2015; Stoney and McCaffery, 2016). Haybaeck et al. (2015) found the brains of patients with SZ, BD, or MDD to have significantly increased expression of vitamin A-inducible or induced gene 1, pointing to altered signaling pathways. Another study found mRNA levels of key elements of vitamin A signaling were significantly reduced in the postmortem dorsolateral prefrontal cortex/anterior cingulate cortex from elderly depressed patients (Qi et al., 2015). A similar signal was detected in a chronic unpredictable mild stress model in rats (Qi et al., 2015). There is evidence of a link between isotretinoin use and depression and suicide (Bremner et al., 2012; Hu et al., 2016), clinical exacerbation of BD, and possibly to psychosis (Ludot et al., 2015). Vitamin A therapy at high doses is also associated with cognitive decline (de Oliveira et al., 2009; 2015) and increased levels of oxidative stress markers in both human and animals (de Oliveira et al., 2009).
Vitamin C is an antioxidant capable of scavenging free radicals and other ROS formed in cell metabolism. In addition to its role as an antioxidant, vitamin C is a co-substrate of many important oxidoreductases and may regulate gene transcription (Arrigoni and de Tullio, 2002). Because of these characteristics, vitamin C has been tested as a possible adjunctive therapy in psychiatric disorders. A double-blind, placebo RCT in high school students showed lower levels of anxiety after 14 days of vitamin C supplementation compared with placebo (de Oliveira et al., 2015). Positive results were also reported in a 6-month, double-blind, randomized control pilot trial with 1000 mg/d vitamin C as an adjunct to 10 to20 mg/d fluoxetine in children (n=24) diagnosed with MDD (Amr et al., 2013). However, the only RCT testing vitamin C as an adjuvant (1000 mg/d) in the treatment of adults (n=43) with MDD (added to 60 mg/d citalopram) showed no statistically significant results (Sahraian et al., 2015).
In BD, vitamin C was proposed as a treatment in a double-blind, placebo control cross-over trial, where 23 BD participants receiving 3 g/d of vitamin C reported improvement in depressive symptoms (Naylor and Smith, 1981). Kay et al. (1984) conducted a 28-day, double-blind, randomized active-control study with 61 BD inpatients (29 with manic symptoms and 32 with depressive symptoms). The depressed participants received either 150 mg/d amitriptyline (n=14) or 4 g/d vitamin C plus 4 g/d ethylene diamine tetra acetic acid (EDTA) (n=18). The manic participants were also divided into 2 groups—13 were medicated with 800 g/d lithium and 16 received only vitamin C plus EDTA. Manic participants responded better to lithium than to vitamin C. There was no significant difference in depression symptoms between amitriptyline or vitamin C in the depressed group on HAM-D and Beck Depression Inventory (BDI) ratings.
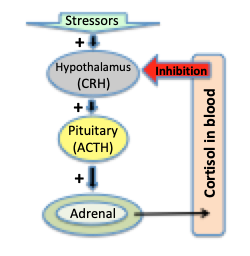
Vitamin D is a fat-soluble antioxidant involved in the regulation of calcium and phosphate metabolism. Moreover, vitamin D is implicated in the production of melatonin and in seasonal affective disorder (Gloth et al., 1999). The association between low levels of vitamin D and mood disorders (MDD, BD, and dysthymia) has been established (Anglin et al., 2013; Belzeaux et al., 2015), and it was also identified as a risk factor for development of postpartum depression in pregnant women (Robinson et al., 2014). Furthermore, vitamin D influences monoamine metabolism by modulating the hypothalamic-pituitary-adrenal axis through vitamin D receptors (VDRs) (Puchacz et al., 1996; Prüfer et al., 1999; Eyles et al., 2005). VDRs also affect nuclear transcription, regulate the expression of the dopamine receptor gene (Trinko et al., 2016), and may also be involved in the regulation of mitochondrial function and lipid metabolism (Silvagno and Pescarmona, 2017). VDR is now known to translocate into mitochondria, which raises the possibility of vitamin D having a direct impact on cellular bioenergetics by altering mitochondrial function and VDR to work as a modulator of energy balance in humans (Silvagno and Pescarmona, 2017). Studies on cancer cells (Consiglio et al., 2014), keratinocytes (Consiglio et al., 2015), adipocytes (Ricciardi et al., 2015), and VDR-null mutant mice (Wong et al., 2011) found that VDR can influence the transcription of proteins of the mitochondria respiratory chain, inhibiting it and redirecting Krebs cycle intermediates toward biosynthesis (Consiglio et al., 2014). However, establishing the treatment effect of vitamin D supplementation has been somewhat problematic as studies are likely too heterogeneous (including depression, seasonal affective disorder, obesity, postmenstrual tension, and hospitalized patients). Therefore, varying the selection criteria wields both positive and negative meta-analysis results: A meta-analysis of 15 RCTs (with samples between 15 and 2117) was favorable for vitamin D supplementation (≥800 I.U. daily) (Spedding, 2014), while another meta-analysis using 6 RCTs (n=1203, 71 depressed) showed no significant effect of vitamin D supplementation on postintervention depression scores (Li et al., 2014). A more recent double-blind RCT of 40 MDD patients on vitamin D monotherapy (50 kIU/d for 8 weeks) showed beneficial effects on the depressive symptoms measured by the BDI on indicators of glucose homeostasis and on oxidative stress levels (Sepehrmanesh et al., 2016). Regarding BD, an 8-week open-label trial tested the effect of adjunctive vitamin D supplementation in mania in young bipolar spectrum disorder patients (aged 6–17 years old). There was a significant decrease in YMRS scores and improvement in levels of glutamate and γ-aminobutyric acid (GABA) measured in the anterior cingulate cortex (Sikoglu et al., 2015).
Vitamin E or tocopherol is a fat-soluble antioxidant, which has a stabilizing function in the mitochondrial membrane attributed to radical scavenging and lipid peroxidation reduction (Kagan et al., 1990; Pham-Huy et al., 2008). Studies have suggested that vitamin E may be more effective when combined with CoQ10 or vitamin C (Kontush and Schrkatolina, 2004; Dhitavat et al., 2005). To our knowledge, the efficacy of vitamin E in BD or MDD has not been examined. Some animal studies found positive results—chronic administration of high doses of vitamin E improved lifespan, neurological performance, and brain mitochondrial function in aging mice (Navarro et al., 2005). Likewise, studies in Alzheimer’s disease are also promising. A multi-center RCT studied the effect of vitamin E supplementation in 613 participants with mild-to-moderate Alzheimer’s disease, medicated with memantine, and reported slower functional decline and decreased caregiver burden (Dysken et al., 2014). A cross-sectional and prospective study of 104 patients with Alzheimer’s disease showed reduced prevalence and incidence of Alzheimer’s on those consuming vitamin E plus C supplementation (Zandi et al., 2004). A clinical trial with combined therapy with vitamin C for MDD in elderly patients is now in the recruiting phase (NCT02793648).
The vitamin B complex contains water-soluble vitamins B1, B2, B3, B5, B6, B7, B9, and B12. They play an important role in a variety of critical brain pathways and participate in mitochondrial energy production and cellular function (Dean et al., 2012). Vitamin B complex is known to influence cognitive performance and mood. Its influence in CNS function has been suggested to occur in 2 interrelated ways: direct via of hypomethylation and indirectly by homocysteine levels resulting in structural changes in the brain (Calvaresi and Bryan, 2001). They often work in synergy and thereby are best administered as a complex (Dean et al., 2012).
Vitamin B9
Vitamin B9, or folate, is involved in the synthesis, repair, and methylation of DNA and in the formation of monoamine neurotransmitters, thus being important in the pathogenesis of affective disorders (Mattson and Shea, 2003; Folstein et al., 2007; Miller, 2008; Sharpley et al., 2014). Together with vitamin B12, vitamin B9 plays an essential role in mitochondrial energy production through 1-carbon transfer pathways (Dean et al., 2015). Folate deficiency has been associated with several neuropsychiatric disorders, especially in inpatients (Hall et al., 1997; Dean et al., 2015) such as depression, BD, and cognitive dysfunction (Bell et al., 1990; Godfrey et al., 1990; Hasanah et al., 1997; Selhub et al., 2000; Bryan et al., 2002; Reynolds, 2002; Gilbody et al., 2007). Furthermore, in long-term lithium-treated patients, low serum folate levels were associated with higher affective morbidity (Coppen and Abou-Saleh, 1982). Schou et al. (1986) also found low levels of folate in untreated BD patients (25% lower than controls) and their normalization after 6 months of lithium. Behzadi et al. (2009) conducted a preliminary RCT with 88 BD type I manic patients treated with sodium valproate and adjuvant folic acid (synthetic form of folate). After 3 weeks, a statistically significant difference in the YMRS was found. Another double-blind RCT of 75 lithium-treated BD patients on a daily supplementation of 200 μg folic acid for 52 weeks showed a significant reduction in affective morbidity (Coppen et al., 1986). L-methylfolate was also recently studied in the first open-label trial for bipolar depression. Ten patients with BD type I on standard treatment for bipolar depression (but with no antidepressant) received 15 mg of folate daily for 6 weeks. A 55% improvement in depression symptom ratings (MADRS) and a small mean decrease in YMRS was found, suggesting its potential as BD adjunctive treatment (Nierenberg et al., 2017). L-methylfolate has potential as an adjunctive treatment for unipolar depression. Two multicenter sequential parallel comparison design trials were conducted with MDD patients (n=148 and n=75) with partial or no response to serotonin reuptake inhibitors. L-methylfolate supplementation was given for 30 days at the dosing of 7.5 mg/d and augmented later to 15 mg/d in the following month in trial one. In trial two, 15 mg/d of L-methyfolate was given for 60 days. The second trial had positive results on primary outcomes—degree of improvement in depressive symptom score and response rate (Papakostas et al., 2012). Folic acid was also found to improve the therapeutic effect of fluoxetine in depressed patients in another 2 placebo-controlled RCTs. Studies with samples of 127 and 42 patients with MDD, respectively, were treated with folic acid plus 20 mg of fluoxetine and showed greater improvement in the HAM-D and in the BDI (Coppen and Bailey, 2000; Venkatasubramanian et al., 2013). Moreover, long-term treatment of post-stroke survivors (n=273) with folic acid, B6, and B12 was associated with a reduction in the risk for MDD (Almeida et al., 2010). The effect of vitamin B9 as a possible early intervention was studied in a double-blind, placebo RCT in healthy teenagers (n=112) with increased familial risk of depression and BD. Folic acid did not reduce the incidence of a mood disorder diagnosis but may have delayed the first mood episode and its clinical presentation tended to be milder (Sharpley et al., 2014).
Vitamin B1
Vitamin B1, or thiamine, functions as a cofactor essential for the oxidative decarboxylation of the Krebs cycle (Depeint et al., 2006). Vitamin B1 deficiency is associated with neurological problems, including cognitive deficits and encephalopathy (Depeint et al., 2006; Gibson et al., 2016). Healthy elderly women with marginal vitamin B1 deficiency experienced with thiamin supplementation a significant increase of appetite, body weight, energy, and activity, and decreased fatigue, improvement of sleep patterns, and of general well-being (Smidt et al., 1991).
Vitamin B3
Vitamin B3, or niacin, is a precursor for NADH and nicotinamide adenine dinucleotide phosphate, which is involved in more than 500 enzymatic reactions pertaining to mitochondrial respiration (oxidative phosphorylation), glycolysis, and lipid oxidation (Depeint et al., 2006). The potential of NADH as an antidepressant was first tested in the FST model in Wistar rats, yielding a similar effect to fluoxetine (Rex et al., 2004). Vitamin B3 supplementation was also shown to prevent development and progression of mitochondrial myopathy in mice (Khan et al., 2014). More relevant to BD, evidence of mood elevation was reported in a 54-year-old man with no previous mental illness, who had a manic episode after commencing vitamin B3 for his dyslipidemia (Loebl and Raskin, 2013).
Vitamin B6
Vitamin B6 refers to 3 primary forms: pyridoxine, pyridoxal phosphate, and pyridoxamine. The last 2 serve as coenzymes for protein metabolism, conversion of tryptophan to niacin, and neurotransmitter function. Some of the protective effect of vitamin B6 may occur via modification of mitochondrial function by preventing the oxygen radical generation and lipid peroxidation (Kannan and Jain, 2004). Higher dietary intake of vitamin B6 and folate was associated with lower prevalence of depression symptoms (measured with the Center for Epidemiologic Studies Depression Scale) in a large cross-sectional study of 6517 community adolescents (aged 12 to 15) (Murakami et al., 2010). Another study in 38 healthy older men on 20 mg of vitamin B6 supplementation showed cognitive benefits such as improved memory but failed to improve mood (Deijen et al., 1992). A double-blind RCT in 211 healthy women showed similar results (Bryan et al., 2002). Another 4-week, double-blind RCT with 14 geriatric depressed inpatients tested the augmentation of tricyclic antidepressant treatment with vitamins B1, B2, and B6 (10 mg/d). The active vitamin group demonstrated greater improvement in scores on ratings of depression and cognitive function (Bell et al., 1992). A 24-week, open-label clinical trial with 10 participants with SZ patients that were already receiving antipsychotics were given 1200–2400 mg/d of pyridoxamine. The patients had high levels of plasma pentosidine, a carbonyl stress biomarker. The results were measured with the Positive and Negative Syndrome Scale score and the Brief Psychiatric Rating Scale. Treatment augmentation with pyridoxamine showed partial results in participants with enhanced carbonyl stress; however, only 3 patients had reduction of psychopathology. Four patients showed improvement on iatrogenic parkinsonism. However, 2 patients had Wernicke’s encephalopathy-like adverse drug reactions, reversed by thiamine supplementation (Itokawa et al., 2018).
Vitamin B2
Vitamin B2 is a precursor of flavin adenine dinucleotide and flavin mononucleotide and is required for electron transport chain in complexes I and II. They work synergistically with other B vitamins for mitochondrial respiration (Depeint et al., 2006). Henriques et al. (2016) showed that vitamin B2 supplementation could functionally compensate for mitochondrial ß-oxidation enzymes. Four nonrandomized trials have been reported effectively treating mitochondrial diseases with complex I and/or complex II (Bernsen et al., 1993; Bugiani et al., 2006; Gerards et al., 2011) and III and IV (Ghezzi et al., 2010) deficiency.
Vitamin B5
Vitamin B5 is the precursor of CoA, important in the Krebs cycle and fatty acid oxidation. In vitro and in vivo studies suggest that vitamin B5 can restore ATP synthesis levels as well as the activity of antioxidant enzymes and can prevent the collapse of mitochondrial membrane potential (Depeint et al., 2006). There are established associations between vitamin B5 deficiency and neurodegenerative diseases, dermatitis, hypoglycemia, convulsions, and encephalopathy with liver failure (Depeint et al., 2006).
Vitamin B7
Vitamin B7 is a coenzyme for 5 mitochondrial carboxylases and is essential for growth, development, and normal mitochondrial and cellular functions, including fatty acid oxidation and gluconeogenesis. Reductions in vitamin B7 result in the loss of mitochondrial complex IV, which leads to increased production of oxidative species by the mitochondria (Depeint et al., 2006). Several clinical disorders are associated with B7 deficiency, such as cutaneous conditions (skin rashes, alopecia, and conjunctivitis), neurological conditions (depression, seizures, paresthesia), and diabetes (Depeint et al., 2006).
Vitamin B12
Vitamin B12, or cobalamin, is a cofactor for methionine synthesis, required for DNA and myelin synthesis and maintenance of neuronal integrity as well as neurotransmitter regulation. Vitamin B12 deficiency is a common but often under-recognized condition causing neurologic, cognitive, psychiatric, and mood symptoms (Lindenbaum et al., 1988; Issac et al., 2015). Further, deficiencies of B12, folate, or B6 can lead to macrocytic or pernicious anemia with symptoms of fatigue, psychomotor, cognitive, and mood deficits (Selhub et al., 2009). In an RCT in elderly participants with depressive symptoms, long-term daily supplementation with folic acid and vitamin B12 improved cognitive functioning, particularly immediate and delayed memory performance (Walker et al., 2012). More relevant to BD, there is a case-report of an acute onset of mania in a 94-year-old man with no previous mental illness and profound cobalamin deficiency who responded to cobalamin therapy (Jacobs et al., 1990). In a double-blind RCT of vitamin B12 supplementation in winter seasonal affective disorder, no significant differences were found (Oren et al., 1994). No benefit for B12 replacement was found in cognitive symptoms in dementia (van Dyck et al., 2009) or depressive symptoms in an elderly man (Ford et al., 2008).
Taurine is a free amino acid that has important functions as a neuromodulator and antioxidant. It protects against glutamate-induced neurotoxicity and has been hypothesized to prevent membrane depolarization and mitochondrial energy failure (Timbrell et al., 1995; Ye et al., 2013). Recently, taurine has been reported to reduce oxidative stress and maintain mitochondrial function in cortical neurons (Xu et al., 2015). Moreover, taurine acts as an agonist for glycine and γ-aminobutyric acid receptors (Albrecht and Schousboe, 2005). In the FST model in rats, taurine supplementation has antidepressant-like effects (Toyoda and Iio, 2013). In a double-blind RCT in people with first-episode psychosis, taurine improved symptoms of depression and reduced psychotic symptoms as well as improved measures of functioning but failed to impact cognition (O’Donnell et al., 2016). While a double-blind RCT in BD adolescents with a manic episode was conducted (CT00391001), the study was terminated and no results have been published. Another double-blind RCT was carried out but despite its completion, no results have been revealed at this time (NCT00217165).
An agonist of the PPAR usually prescribed as an hypolipidemic drug, bezafibrate can restore fatty acid oxidation activity in cells from carnitine palmitoyltransferase-2 and very-long-chain acyl-CoA dehydrogenase deficiencies in in vitro conditions (Bastin et al., 2008). Data suggest that the PPAR signaling pathway is directly implicated in mitochondrial physiology. Exposure to bezafibrate increased the transcription of HADHA and HADHB genes (responsible the encoding of alpha and beta subunit of the mitochondrial trifunctional protein) (Aoyama et al., 1998), immune-detectable alpha and beta subunit proteins, activities of long-chain 3-hydroxyacylCoA dehydrogenase and long-chain 3-ketoacylCoA thiolase, and stimulated fatty acid oxidation capacities in human fibroblasts (Djouadi et al., 2016). To the best of our knowledge, no clinical data are available in the literature regarding the role of benzafibrate in psychiatry. However, an 8-week, open-label pilot trial of bezafibrate 400 mg/d added to lithium in 20 participants with bipolar depression is being conducted to assess its safety, tolerability, and antidepressant efficacy (NCT02481245).